From Treating Trapped Nerves Home Study
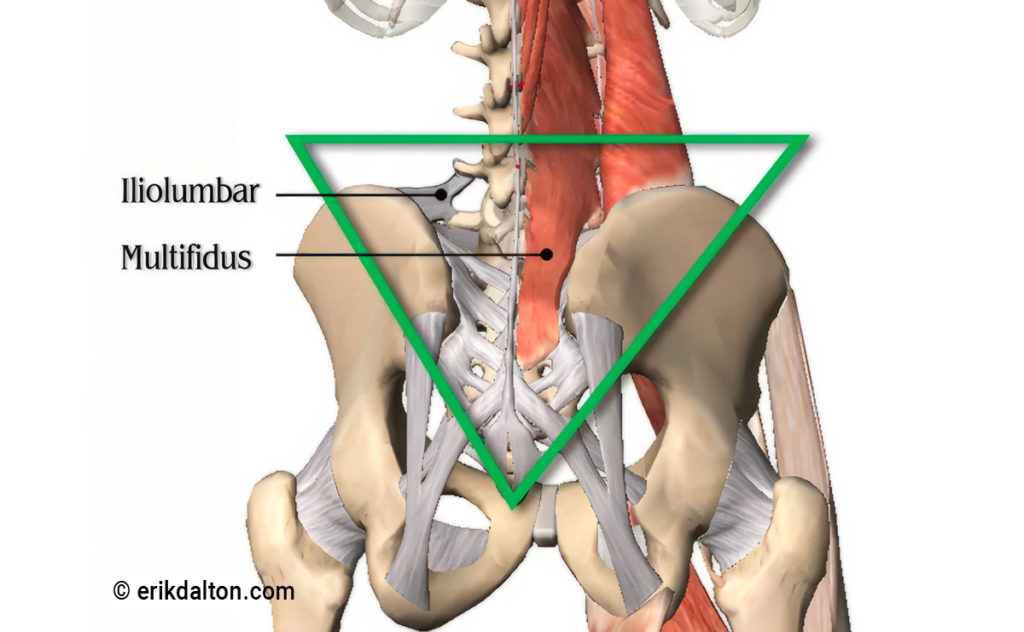
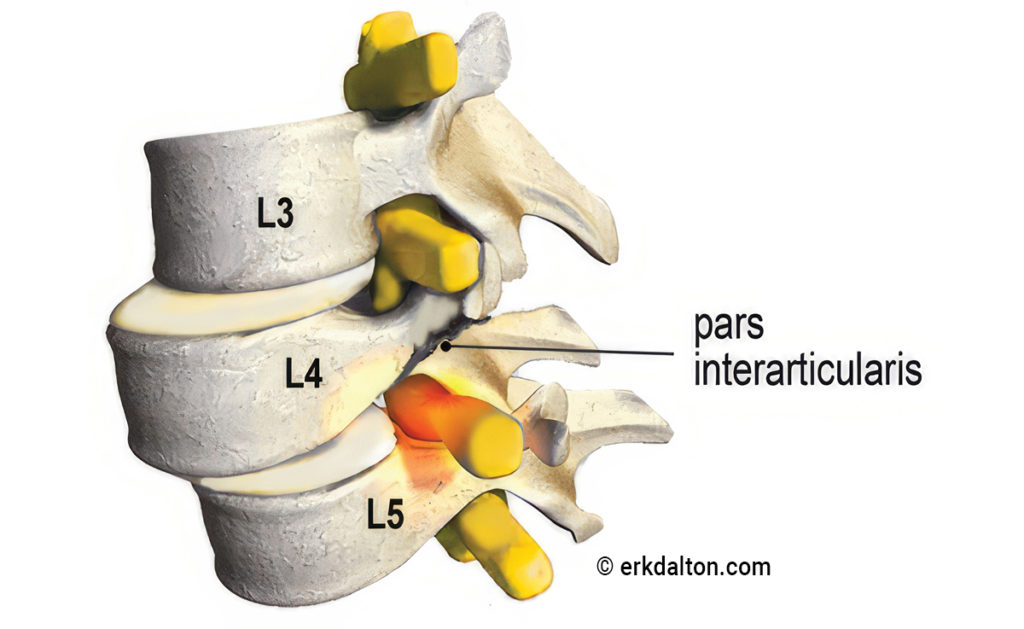
The primary role of the iliolumbar ligaments is to prevent excessive lumbar sidebending, but these ligaments can contribute to sciatic nerve entrapment when injured. A traumatic event such as a bending and twisting maneuver while attempting to lift a heavy object, may strain the iliolumbar ligaments and their multifidi neighbors (Image 1). As the ligaments weaken, they lose the ability to prevent the fifth lumbar vertebra from shifting forward on the sacrum which may cause contralateral narrowing of the intervertebral foramen, facet arthrosis and possible sciatic nerve entrapment. Corrective exercises such as planks and bird-dogs may, in time, restore strength and stability to these stretch-weakened ligaments, and I have had some success using fast-paced, low-force “scrubbing” to help tighten the injured ligaments via enhanced hydration and fibroblastic proliferation (Image 2). In extreme cases, slippage of the fourth or fifth lumbar vertebra may result in spondylolisthesis, where the pars interarticularis cracks from excessive pressure, allowing sciatic nerve entrapment on one or both sides (Image 3).

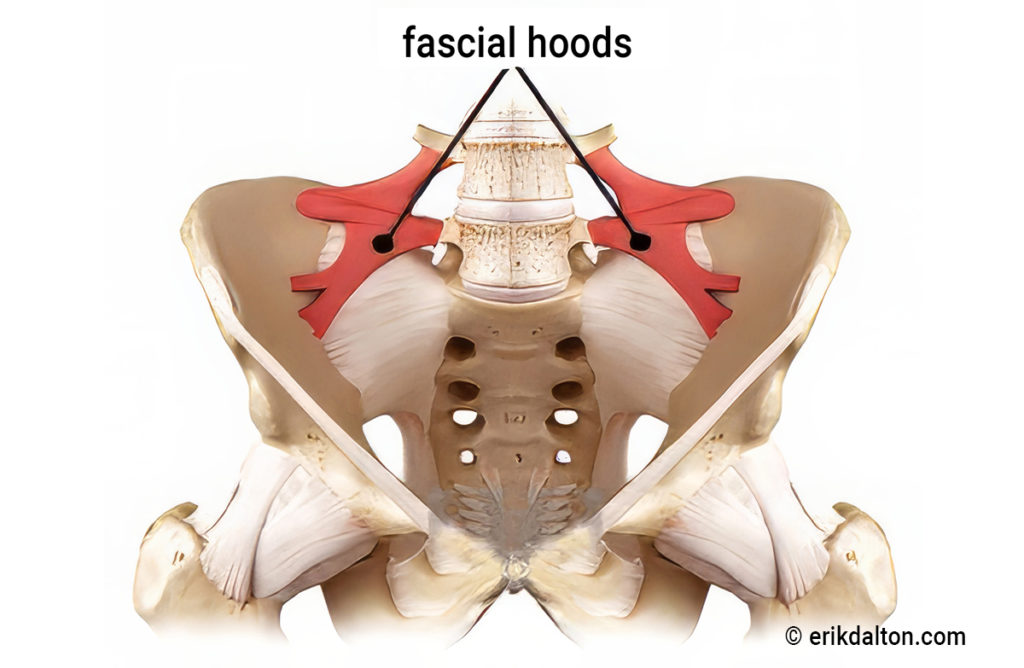
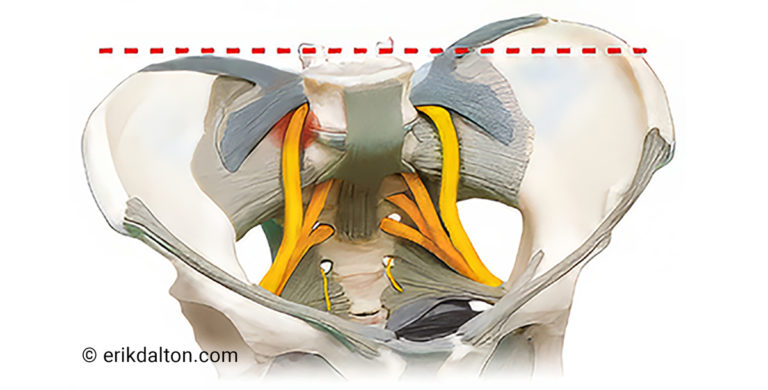
Yet, one of the lesser-appreciated areas for sciatic nerve occlusion lies beneath the anterior iliolumbar ligaments. First discovered by famed anatomists Drs. Philip Hanson and Bill Sonesson, notice in Image 4, how these taut bands on the anterior surface form “fascial hoods” over the L4 and L5 nerve roots.1 Once the greater sciatic nerve (about the size of your pinky finger) leaves the spine, it must traverse through these taut bands. In a nicely aligned pelvis, this usually presents no compression problems. But visualize how a torsioned pelvic bowl could bind the anterior iliolumbar ligaments against the pelvic bowl occluding the underlying sciatic nerve roots (Image 5).
In the beginning, the client may or may not experience symptoms depending on the brain’s perception of the degree of threat. However, prolonged nerve root compression may begin to obstruct axoplasmic transport of proteins and other cell parts to and from the neuron’s cell body. Clinically, this breakdown of nerve conduction may lead to what Harvard University plastic surgeons Albert Upton and Alan McComas called “double crush syndrome.”2 This term refers to scenarios where compressed axons at one site cause the nerve to become especially susceptible to damage at another site, such as under the piriformis muscle.
The brain may try to stabilize the lumbosacral joint by layering the area with protective multifidus muscle spasm, but it does little good to try to release hypertonic spasm in these spinal groove stabilizers until the pelvic alignment problem is corrected. Fortunately, there are many ways manual therapists can successfully assess and correct iliosacral alignment, yet the technique shown in Image 6 is one of my favorites.

References:
1. P. Hanson and B. Sonesson, “The Anatomy of the Iliolumbar Ligament,” Archives of Physical Medicine & Rehabilitation 75, no. 11 (November 1994): 1,245–46.2. A. R. Upton and A. J. McComas, “The Double Crush in Nerve Entrapment Syndromes,” Lancet 2, no. 7,825 (August 1973): 359–62.
On sale this week only!
Save 25% off the Upper Body Course!
NEW! Enhanced video USB format!!!
Learn unique approaches to work with the shoulder girdle, arms, neck, and torso, this course will prepare you to relieve painful myoskeletal issues in the upper body. Through video demos and animation, you’ll learn to identify several compensatory movement patterns and their associated reflexogenic pain. With this understanding of where the true source of problems arise, you’ll be able to develop highly effective treatment protocols and deliver lasting results. This course provides you with the skills you need to confidently relieve pain issues in the upper body. (20 CE)
Bonus: When you order the Home Study version, get the eLearning course and and an additional 2CE Ethics eCourse for free!
Save 25% off the Upper Body Course this week only. Offer expires Sunday, March 1st. Click the button below for more information and to purchase the course for CE hours and a certificate of completion to display in your office.








