This is part 3 of a three-part article series on Massage Therapy Myoskeletal Alignment Techniques running in Massage Magazine’s 2002 January/February, March/April and May/June issues.
Introduction
Famous for their amazing ability to precisely define complex anatomical structures, the early Greeks hit the nail on its proverbial head when they labeled dura mater, the “tough mother.” Centuries later, massage therapists have come to understand the important role dura mater plays in protecting the brain and spinal cord. Interestingly enough, many therapists are surprised to learn that a variety of common neck, head and low-back complaints actually originate from distortion of this sensitive membrane.
Dural torsioning, compression and impingement often result in mysterious pain patterns that can mimic muscle spasm. If the dural tube is both overstretched and twisted from myofascial contractures, bony misalignment or spinal pathology, complex conditions such as migraines, sciatica, thoracic outlet syndrome and scoliosis can manifest. Sadly, these pain generators offer a major therapeutic challenge to today’s body worker who relies exclusively on conventional myofascial modalities to help clients who present with these conditions.
As students of an evolving, health-conscious society, massage therapists will reap fruitful rewards by incorporating specific techniques to maintain the delicate balance of tone and tension in the body’s dural system. But to learn, one must always begin by investigating the rudimentary workings of this elaborate mechanism. For example, how does the dural system operate? And more importantly, what tools are available for today’s body worker to help restore function once this sensitive membrane has been strained? Hopefully, answers to these and other questions can be gleaned from a general discussion of basic scientific information regarding this intriguing subject.
The Toughest Envelope
First and foremost, one must remember that the dura is the toughest, outermost envelope enclosing the central nervous system, and the most fibrous of the three protective membranes. Two of the dural layers are complexly arranged within the skull and help form the craniosacral pumping mechanism. With several attachments to cranial structures, including the occiput, temporals and sphenoid bone, the dura loves its “free-floating” mobility within the cranial vault and is happiest when sliding freely up and down within the spinal canal (see Figure #1).
As a suspension bridge spans across a river or bay, the brain and spinal cord are suspended within the skull and vertebral column by tooth-like denticulate ligaments that connect the brain and cord with the dura mater. The tough dural covering is loosely bound to specified places inside the cranium.
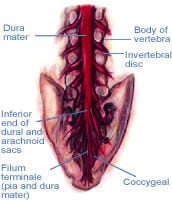
Figure #1: The dura mater. If the dural tube is both overstretched and twisted from myofascial contractures, bony misalignment or spinal pathology, complex conditions such as migraines, sciatica, thoracic outlet syndrome and scoliosis can manifest.
As it makes its descent downward, firm attachments bind it to only a few places along the bony vertebral column-the posterior bodies of the second and third cervicals (C2 and C3), the second sacral segment, and the most inferior vertebra of the spine, the coccyx.
The head, spine and all related myofascial structures are designed for constant movement and motion that simultaneously change the shape of the dura mater. Because the layers are plicated, or folded like a fan, the dura has the ability to slightly elongate.
For years cranial researchers, such as John Upledger, D.O., have observed and reported on the effects this changing dural tension engenders on the human nervous system and the systemic health of the individual as a whole. When the dura is stretched, compressed, torsioned or distorted by the moving of bones attached to it, the spinal cord and brain alter their shape, as well. In turn, this action overtly expresses itself by changes in intensity, frequency and the amount of nerve flow to and from the brain.
An excellent example of how misaligned bones create adverse dural tension and peculiar pain syndromes is commonly found at the second cervical vertebra: the axis.
The Axis, Suboccipitals, and Head Pain
Because of its direct attachment to the dural tube, poor alignment at C2 frequently becomes a major source of head and neck pain. In the embryo, the rod-shaped notochord develops at the axis. It is the center of development of the axial skeleton and instrumental in determining the final construction of the nervous system; therefore, therapists must appreciate this area as the body’s premiere neurological and biomechanical center.
When the axis is properly aligned, and the dural membrane is not overstretched by cranial or sacral asymmetries, all is well. But when the facet joints of C2 and C3 are jammed together and refuse to open on one side, the vertebra rotates to the side of the fixation and drags the dura with it. This condition alone can cause local pain and reduced range of motion during head flexion and rotation.
However, when a rotated axis combines forces with an already overstretched dural tube from cranial or sacral distortions, a full-blown central nervous system assault suddenly transpires. To relieve the client’s agonizing symptoms and restore healthy functioning, massage therapists must first understand how the axis becomes misaligned and which techniques work best for releasing the disgruntled dural membrane.
The axis is considered the most important cervical vertebra, partly due to its unique dural attachment and also because of the powerful myofascial structures anchoring it from above and below. Deep suboccipital muscles that bind C2 to the occiput and atlas work in harmony with other muscles to balance the head on the neck.
When a forward-head posture develops from prolonged sitting, the lower cervical vertebrae slide forward on the upper thoracics. The unrelenting force of gravity pulls the head down and one finds himself looking at the ground. Of course, the brain unconsciously revolts by immediately recruiting the suboccipitals and other head-extensor muscles to help level the eyes. Make no mistake, the brain will level the eyes against the horizon even if it means ravaging the neck.
Therapists can easily locate the C2 spinous process by palpating for the inferior bump on the occipital bone. By sliding the index finger inferiorly, a soft gap is felt. This is where the spinous process of the atlas would be if left to Mother Nature. The very next bone palpated as the finger moves inferiorly is the spinous process of the axis (flex and extend the head for easy identification). The therapist must be able to quickly locate this bony prominence to accurately assess and release three extremely important suboccipital muscles responsible for atlas/axis misalignment, forward-head posture and pain caused by “dural drag.”
Figure #2: Suboccipital muscles. Deep suboccipital muscles that bind C2 to the occiput and atlas work in harmony with other muscles to balance the head on the neck.
Although six of the eight suboccipitals rotate, side-bend and tilt the head back into hyperextension, the rectus capitis posterior major and minor are the primary offenders in forward-head postures and nagging headaches (see Figure #2). When hypertonic and short, the recti muscles join forces with the sternocleidomastoid and head extensors to slide the occiput forward on the atlas through the occipital condyles.
To palpate and release tight recti muscles, place the client in a left side-lying position and slide the right thumb superiorly and slightly laterally from the axis to the rectus capitis major attachment at the occiput. Place the left thumb beside the right thumb so that it contacts the client’s right rectus capitis minor (see Figure #2). Then allow the fingers of both hands to comfortably drape the client’s head. The client takes a deep breath to a count of five while gently cocking her head into hyperextension against isometric resistance from therapist’s thumbs and hands. On exhalation, the thumbs slowly bring the head into more flexion. Repeat this three times and perform the same technique on the opposite side.
Known as the most innervated of all spinal muscles, the suboccipitals revolt angrily against sustained isometric contraction from prolonged sitting, reading, computer work and general inactivity. When subjected to these stressors, the rectus capitis major and minor eventually fibrose, shorten and compress sensitive neural and vascular structures. As muscles and joint capsules accumulate toxic waste products from lack of motion, irritated chemoreceptors and nociceptors begin to fire noxious messages to the spinal cord, causing the brain to “lock down” the area with protective muscle spasm. The result: cervical stiffness, head pain, dizziness, loss of range of motion and, sometimes, vertigo-like symptoms. Furthermore, as the occiput slides forward on the atlas from hypercontracted recti muscles, blood flow from the cranium can become restricted. Pressure build-up from lack of adequate venous drainage causes trapped blood to collect and compress certain cerebral areas. Soon the client feels the first signs of painful, pounding vascular headaches that frequently hurt in one particular spot as inter-cranial pressure rises.
In many clients, fibers of the rectus capitis minor penetrate the foramen magnum attaching directly to cranial dura mater. If weak and flabby, they do not function as an adequate anchor for the dura during flexion movements. When tight and short, headaches begin as fibers of the rectus capitis minor drag on the dural membrane, interrupting cerebrospinal fluid flow.
Oddly enough, their primary function doesn’t seem to be head hyperextension. Phillip Greenman, D.O., and others have observed that these tiny suboccipitals prefer to fire at the end range of head flexion. It is believed that this reaction is a protective device for securing the dura during whiplash-type motions. Regardless, to restore proper function, these highly specialized muscles must be lengthened if fibrotic or tonified if weak and flabby.
Stomach-Sleepers
The typical “stomach-sleeper” turns his head to one side in order to breathe. Normally the head is turned to the dominant side (usually the right). Since the inferior oblique muscle is the primary head rotator (atlas on axis), prolonged stomach sleeping with the head turned right slackens this muscle over time. Meanwhile, the inferior oblique on the left becomes overstretched and weak. As the client continues sleeping with the head turned right, the muscle ends are brought closer together, increasing tonus in the right inferior oblique. Suddenly one morning the client rises and begins to straighten the head. Shooting pains cause a frantic call to his therapist-simply because the short right inferior oblique prevents the atlas from rotating back left into its normal position on the axis.
As time passes, the atlas becomes fixated in a right-rotated position in relation to the axis. Any attempt to look left forces the axis to rotate left, jamming the C2-3 facet joints together on the right. The axis can become chronically fixated in a left-rotated position, forming that familiar knot massage therapists commonly palpate in the upper left neck. With the atlas rotated right and C2 facet stuck rotated and side-bent left, the torsioned dura loudly rebels. Additionally, if the dural tube is already overstretched from a hooked coccyx, backward sacral torsion, forward-head posture or cranial deviations (particularly occiput and sphenoid), pain, nervous tension and sometimes weird scoliotic patterns appear. Dural strain from longitudinal tensional forces pulling from either end, sphenoid or coccyx, causes neurological pathways leading to and from the brain stem to become disorganized, hyper-excited and overly agitated.
Heartbeat Headaches
The typical stomach-sleeper’s headache throbs and pounds around the ear and temporal bone with each beat of the heart. Fortunately, pain from unilateral temporal headaches is usually easy to relieve using the two-step Myoskeletal Alignment Technique protocol. “Heartbeat headaches” gradually develop as the vertebral artery is stretched and compressed as it threads through the transverse processes of the misaligned atlas/axis and tucks into the foramen magnum.
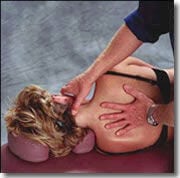
Figure #3: Inferior oblique release, step one: The therapist’s right thumb contacts the C-2 spinous process and slides superio-laterally toward the atlas transverse process while the fingers gently brace the side of the client’s face. The client is asked to inhale to the count of five while gently rotating her head right. The therapist’s right fingers isometrically resist this effort (the therapist’s thumb should feel the inferior oblique tighten). As client exhales, the therapist maintains sustained thumb pressure as the client’s head is slowly turned to the left. The post-isometric relaxation response that follows allows the fibrotic oblique muscle to soften and stretch. Repeat this three times and re-test the atlas’ ability to left-rotate on its axis.
To correct this ornery dysfunction, the client is placed in a left side-lying position, and the therapist begins by contacting the axis spinous process (see Figure #3). The therapist’s right thumb slides laterally toward the atlas transverse process while the fingers secure the right side of the client’s face. As she gently attempts to right rotate her head against the therapist’s resistance, the short, fibrotic oblique capitis inferior (inferior oblique) muscle will “pop up” into the palpating thumb. One or both thumbs may be used to lengthen this short, tight inferior oblique and begin the first step in de-rotating the atlas on the axis. It is easy to see how dural drag from a misaligned atlas/axis can cause pain by irritating this sensitive piezoelectric dural membrane and interrupting cerebrospinal fluid flow.
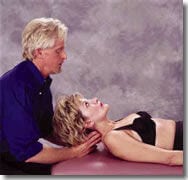
Figure #4: Atlas/axis dural release, step two: With the therapist seated or standing and elbows resting comfortably on a table, extended fingers or thumbs slowly flex the client’s head and neck 45 degrees. The therapist’s right index finger braces the right transverse process of the atlas while his left index and middle fingers contact the left rotated C2-3 joint in the lamina groove. With the client’s head slightly hyperextended, the therapist’s fingers maintain constant pressure as the client slowly chin-tucks while slightly rotating her head to the right. This maneuver rotates the atlas right while releasing the fixated left C2-3 facets. Repeat this three to five times and re-check the atlas/axis alignment.
Step two for correcting heartbeat headaches is demonstrated in Figure #4. As the client slowly performs chin-tucks while right-rotating her head against resistance from the therapist’s extended fingers, adherent facets at C2-3 are released, allowing the atlas and axis to rotate into proper position. Bodyworkers will find this simple two-step procedure for restoring function to the upper cervical complex extremely useful in clients suffering unilateral, pulsating temporal headaches.
Two other remaining spinal structures responsible for head and back pain also merit special attention due to their profound effect on the dura mater: the coccyx and sacrum.
The Hooked Coccyx
The hooked and side-bent coccyx are two of the most devastating and often overlooked spinal dysfunctions. When this tiny group of bones “hooks” anteriorly or side-bends to one side (usually the left), the dural tube tightens (see Figure #5). There are reported cases where a hooked coccyx actually shuts down the entire central nervous system by changing the shape of the piezoelectric gel in the brain and spinal cord, thus hindering cerebrospinal fluid flow.
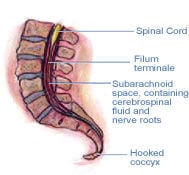
Figure #5: A hooked coccyx. The hooked and side-bent coccyx are two of the most devastating and often overlooked spinal dysfunctions. There are reported cases where a hooked coccyx actually shuts down the entire central nervous system by changing the shape of the piezoelectric gel in the brain and spinal cord, thus hindering cerebrospinal fluid flow.
Strange idiopathic head and low-back pain syndromes frequently manifest when a distorted coccyx tugs on the dural tube, causing reverberating tensional forces to travel all the way up to the occiput. Recurrent, persistent headaches can also develop as a hooked or side-bent coccyx reciprocally alters the position of the sphenoid bone. Difficulty sitting for any length of time, problems with sex, urination, PMS, bed wetting, digestion and extreme sensitivity to light also raise red warning flags of possible coccyx dysfunction.
Ida Rolf, Ph.D., who always referred to the coccyx as the “seat of the soul,” insisted on correcting the hooked and side-bent coccyx during her famous session six of the Rolfing series.
A modified version of Rolf’s coccyx technique is demonstrated in Figure #6. An important note to therapists treating coccyx dysfunction: Always ask the client’s permission to perform this technique due to possible physical and emotional hypersensitivity in the area. Before performing any type of coccyx work, take time to clearly explain what you’re doing and the desired outcome. This ligament-release work shown in Figure #6 should always be performed through underwear or draping.
Addressing a misaligned coccyx can cause the client to become very emotional, due to the vertebra’s direct attachment to the dural membrane by the filum terminale, a long, slender connective tissue strand that terminates at the end of the spinal cord. Connective tissues called the filum durae spinalis enclose the end of the spinal cord and attach it to the deep dorsal sacroccygeal ligament. Low-back, hip and head pain can manifest as the sacroccygeal ligament anteriorly flexes the coccyx, compressing the sensitive filum terminale.
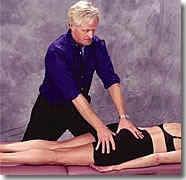
Figure #6: Sacrotuberus/ sacrospinous/ lateral sacrococcygeal ligament release. The therapist releases tight right pelvic ligaments by reaching across the client’s body and contacting the left ischial tuberosity with his dominant thumb and sliding up and under attachments at the inferior border of the sacrum. The therapist’s other thumb braces on top, maintaining sustained upward pressure to release ligaments and gently lift the coccyx from its hooked position. Two minutes of light-to-moderate, fast-paced fibroblast-frictioning helps promote collagen formation in weak, overstretched ligaments. Check the position of the coccyx. If left side-bent, repeat this procedure to short ligaments on the left to restore symmetry.
A hooked coccyx could also lead to loss of psychological integrity. In fact, some reported cases cite severe emotional disturbances in people whose coccyx has been removed or broken off, leaving no anchor for the dura mater.
The coccyx has also been implicated in clients presenting with functional and structural scoliotic patterns. Through its connection with the sphenoid, excessive dural tension stresses the 11th cranial nerve, which, in turn, shortens specific neck and shoulder muscles, including splenius cervicis and levator scapulae. Protective muscle spasm from bilateral dural irritation can compress the C7-T1 area, resulting in dowager’s humps and osteoarthritic bone degeneration, while one-sided dural torsioning forces the cervicothoracic vertebrae to buckle into a scoliotic curve.
Regrettably, the neck and coccyx are not the only structures affected by adverse dural tension. Bodyworkers regularly deal with clients returning week after week, complaining of generalized low-back or sciatic-type pain. Myofascial therapy offers only temporary relief for those clients whose dural tube has been distorted by sacroiliac dysfunctions. This condition is easily recognized due to chronic, sympathetic muscle spasm that stubbornly refuses to release.
Standing Back Pain
Clients complaining of low-back pain from prolonged standing usually suffer various forms of sacroiliac dysfunctions. Among the 10 ways the sacrum can become stuck “crooked” between the two iliac bones, the most common is called a “left unilateral flexed sacrum.” In these clients, prolonged standing forces the left sacral base to move anteriorly/inferiorly and get stuck there.
This aberrant sacroiliac problem often prevents the left facet joints at L5 and S1 from closing during prolonged standing, leading to generalized hip and back pain. For some odd reason, 95 percent of all unilateral flexed sacrums are on the left. Unlike painful sciatic-like sacroiliac dysfunctions, such as backward sacral torsions, the unilateral flexed sacrum can ache deeply on both sides of the low back the longer the client stands. This is primarily due to sinuvertebral nerve innervation of the dura and joint capsule at L5-S1.
To assess this dysfunction, therapists simply palpate both sacral bases, checking for differences in depth. If the sacrum is deep on the left, it is rotated to the right. By sliding the thumbs down to the inferior lateral angles of the sacrum, the therapist can determine which side is most inferior. If the left inferior lateral angle is more inferior than the right and the left sacral base is deep, the sacrum is probably dragging on the left end of the dural membrane, causing the aching back. The myoskeletal contract/relax technique for a left unilateral flexed sacrum demonstrated in Figure #7 is successful in correcting this prevalent chronic back-and-hip complaint.
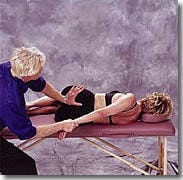
Figure #7: Addressing the left unilateral flexed sacrum. With the client lying on her right side (knees and hips flexed), the therapist grasps the client’s left wrist with his right hand. The therapist’s left palm contacts the inferior left sacral border just above the coccyx. A slow, sustained counter-force is established between his two hands as he gently pulls on the client’s left arm while his left palm braces at the sacrum. The client is asked to inhale and hold to a count of five while gently pulling her left arm against therapist’s isometric resistance. As the client exhales, the therapist takes up the slack by lightly pulling on the client’s arm while maintaining constant pressure on the inferior sacral angle. Anterior/superior palm pressure to the inferior lateral angle of the sacrum causes the left sacral base to move posteriorly into its proper position. Additionally, the stuck facets at L5-S1 are encouraged to close as the pull from the therapist’s right hand left-rotates the client’s trunk. Repeat this three to five times and re-check for sacral base symmetry.
Therapists should remember that most sacroiliac dysfunctions are associated with muscle imbalances in the psoas, piriformis, biceps femoris and weak gluteals. Because fibers of the biceps femoris muscle often originate at the sacrum instead of the ischial tuberosity, hypercontraction of these lateral hamstrings produces a constant drag on the sacrum, dura and the entire pelvic girdle. Therefore, the first step in relieving sacroiliac dysfunction is to balance all muscle groups attaching to the pelvis from below and above.
Obviously, some of these muscles need lengthening while others require restoration of tone. Once myofascial balance is established in the muscles attaching to the pelvis, assessment and correction of any bony restrictions distorting the dural membrane can then be addressed.
Turning Challenge into Triumph
Since the nervous system directs all the body’s functioning, its immediate condition is expressed by the changing of frequency, intensity and quality from the cerebral hemisphere through the spinal cord to the rest of the body. Surprisingly, there are only a few places where the nervous system can be properly tuned, and these “adjusting knobs” are the bones that directly attach to the dura mater.
This article’s focus has primarily centered around the negative effects spinal fixations (axis, sacrum and coccyx) have on the dura mater. The omission of the enormous role cranial dysfunctions play in creating adverse dural tension is intentional. Hands-on approaches for addressing these separate yet equally disturbing conditions can best be learned by attending courses devoted exclusively to this very timely and rewarding body of work.
Faulty alignment or fixations in any bone of the cranial vault or spine will over-stretch, torsion, deform or drag on the dural membrane, disrupting its ability to send or receive reliable signals from musculoskeletal and visceral structures. Since these aberrant dural stresses frequently manifest as spasm and pain, they are often misinterpreted as muscle problems. This is but one reason why therapists will greatly benefit from the ability to quickly distinguish between common myofascial pain syndromes and true adverse dural tension signs. Long-standing pain often fades in memory as dural techniques are properly addressed through training programs devoted to this intriguing area of bodywork. Clients and therapists alike will appreciate the psycho-social-physical contribution of this holistic approach to pain management.
Through the centuries, technological advances and exhaustive research have verified the early Greeks’ amazing understanding of the dura mater’s integral and pervasive role in optimum central nervous system functioning. All somatic therapists will be graciously rewarded by investigating, through formal hands-on training, the awesome effects of this “tough mother” and its profound significance in protecting the brain and spinal cord.
By developing a comprehensive understanding of the internal dynamics of how routine neck, head and low-back complaints originate from this sensitive membrane, today’s massage therapist can turn a therapeutic challenge into triumph by adding dural techniques to their toolbox of touch.
Please note: This article and the accompanying graphics are not a substitute for hands-on training. Readers are urged to seek training and/or to self-assess to make sure they have sufficient education and experience to understand the information presented here and to safely perform the techniques described
On sale this week only!
Save 25% off the Upper Body Course!
NEW! Enhanced video USB format!!!
Learn unique approaches to work with the shoulder girdle, arms, neck, and torso, this course will prepare you to relieve painful myoskeletal issues in the upper body. Through video demos and animation, you’ll learn to identify several compensatory movement patterns and their associated reflexogenic pain. With this understanding of where the true source of problems arise, you’ll be able to develop highly effective treatment protocols and deliver lasting results. This course provides you with the skills you need to confidently relieve pain issues in the upper body. (20 CE)
Bonus: When you order the Home Study version, get the eLearning course and and an additional 2CE Ethics eCourse for free!
Save 25% off the Upper Body Course this week only. Offer expires Sunday, March 1st. Click the button below for more information and to purchase the course for CE hours and a certificate of completion to display in your office.








