As massage therapists, we know that physically active people are less prone to chronic musculoskeletal pain problems. As I like to say, “Motion is lotion.” We must pull and stretch muscle and fascia through movement if we want these tissues to remain elastic, hydrated, and healthy.
What many massage therapists don’t always consider is the importance of mobility to the health of our nervous systems. Nerve fascicles, like muscle fascicles, are wrapped in layers of connective tissue that can stiffen, adhere and become ischemic if we don’t move and stretch them regularly through active movement. And like tight muscles, restricted nerves can cause various problems leading to pain and dysfunction. Therefore, when a client comes to us with a complaint, we have to be able to mobilize nerves as effectively as we mobilize muscle.
Neurodynamics is a term coined by physical therapists David Butler and Michael Shacklock to describe manual methods for mobilizing peripheral nerves.1 Nerve mobilization includes nerve gliding and nerve tensioning. Nerve gliding, or “flossing,” is a manual technique where a therapist uses specific body positions and movements to pull a nerve back and forth along its path, similar to the action of dental floss in tooth care. Nerve tensioning elongates a nerve by placing it under gentle tensile force at both ends. When therapists use these techniques during a massage session, they passively move some areas of the client’s body while the client actively moves others to elicit the proper glide or tension on a nerve. In addition, many therapists teach clients to move their bodies in ways that mobilize the nerves as part of home-retraining exercises to maintain the positive results achieved during sessions.

We can incorporate nerve mobilization methods with massage and other manual therapy techniques to help resolve common soft-tissue conditions like carpal tunnel, thoracic outlet syndrome, hip pain, piriformis syndrome, and more. Unfortunately, while physical therapists, occupational therapists, and athletic trainers use these procedures to increase the efficacy of treatment outcomes, many MTs have never learned these techniques.
In this blog, I’ll introduce neurodynamics and nerve mobilization methods and encourage you to seek training if you find yourself interested in learning more. Nerve mobilization is advanced work requiring proficiency in anatomy, palpation, and client communication.
A System Designed to Move
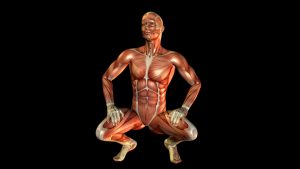
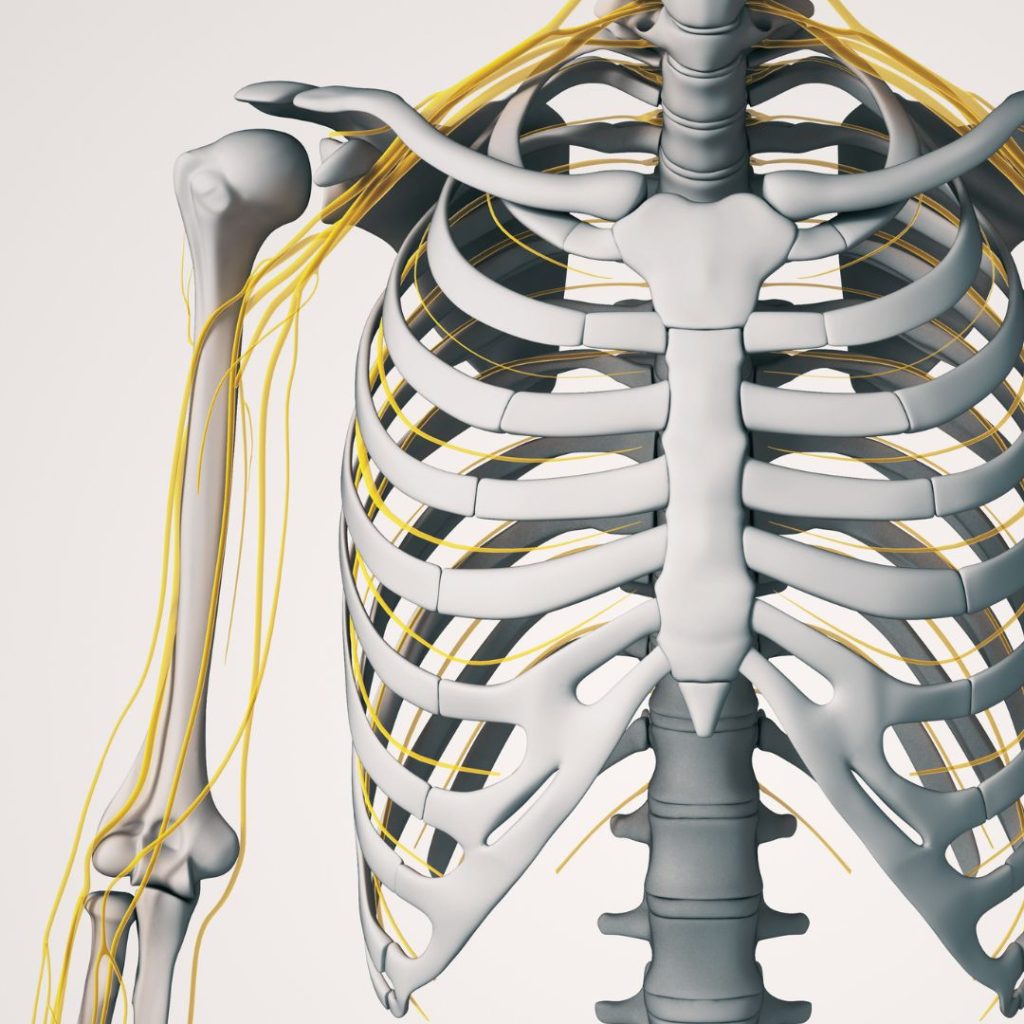
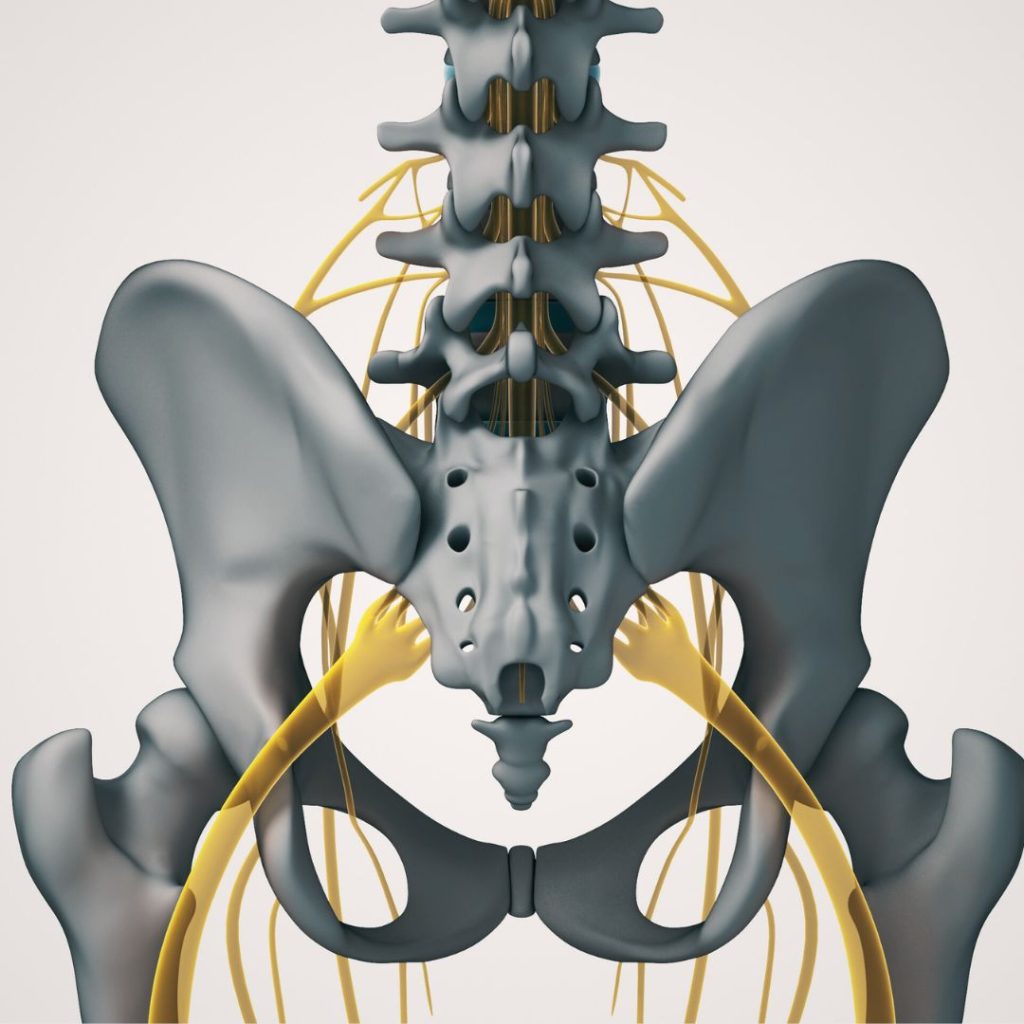
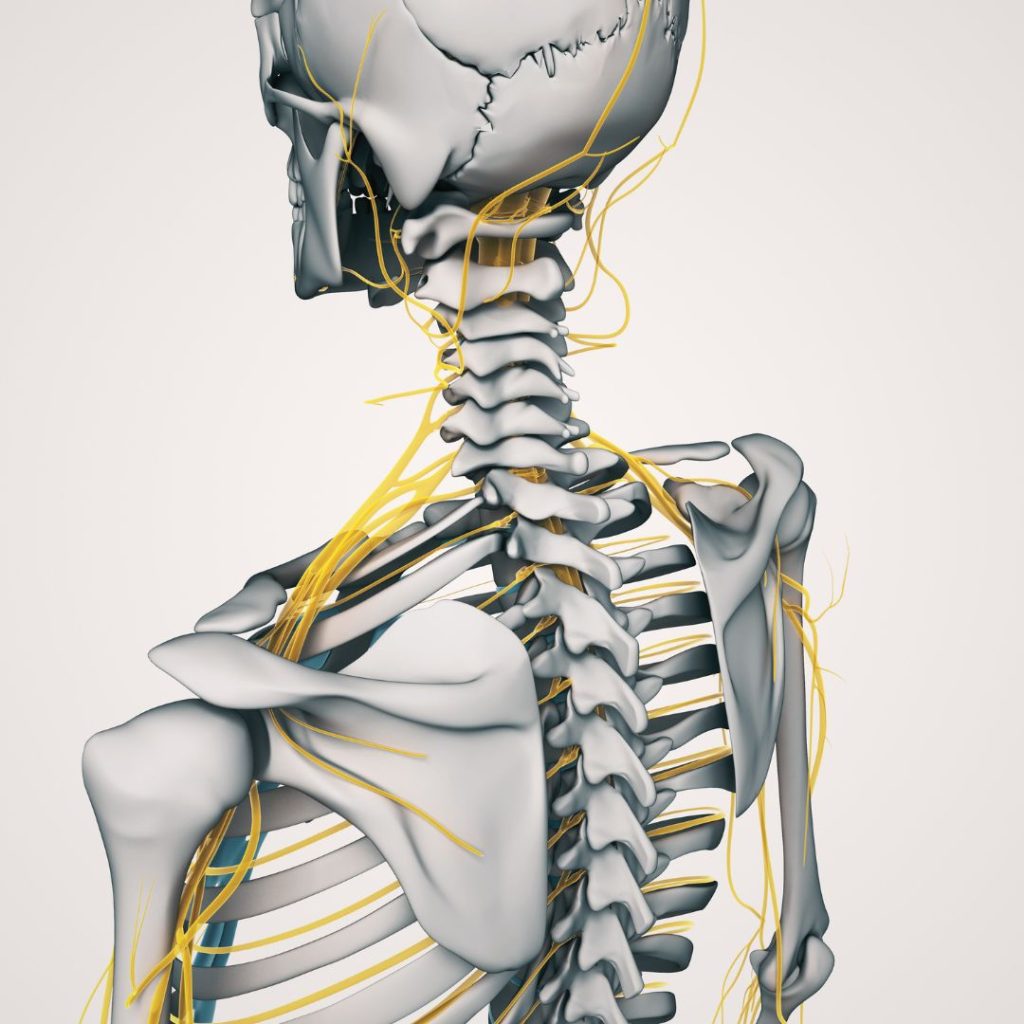
We know that the peripheral nervous system (PNS) relays information between the brain and body through 12 pairs of cranial nerves and 31 pairs of spinal nerves. The structure of a peripheral nerve consists of axons insulated with loose connective tissue, fibroblasts, a few mast cells, macrophages, and endoneurial fluid bundled together and protected by three connective tissue layers – the endoneurium, the perineurium, and the epineurium. Similar to the structure of muscle tissue, axons, Schwann cells, and endoneurial components are bundled by a covering of perineurium to form a nerve fascicle. Epineural tissue wraps several fascicles together to form a nerve.
Scientists presenting a recent model of peripheral nerve structure point out that nerve fascicles are lubricated and designed for independent sliding within their connective tissue coverings. Furthermore, the layers of the endoneurium, perineurium, and epineurium join through viscoelastic connections allowing axons to glide and stretch throughout the length of the nerve. Peripheral nerves can elongate while maintaining the structural integrity of the delicate axons within.2
Nerve Strain and Pressure
We’ve learned that the design of peripheral nerves allows them to withstand significant amounts of nerve elongation, bend and twist during movement. However, imagine how nerve strain increases when a nerve must adapt to additional stress caused by faulty posture, altered joint position, and repetitive strain.
With the initiation of limb movement, a nerve elongates first at the nerve segment adjacent to the moving joint. As limb movement continues, elongation occurs at nerve segments that are progressively more distant from the moving joint.3 At any point along the path of a nerve, muscle, connective tissue, bone, blood in the nerve bed, scar tissue, or inflammation can tether a nerve segment placing it under greater tensile stress. Depending on the circumstances, the nerve might be damaged or irritated, leading to inflammation that creates an anatomical bottleneck or squeezes the nerve and surrounding blood vessels, impairing microcirculation.4
Harvard University plastic surgeons Albert Upton and Alan McComas coined the term double crush syndrome. They state, “Neural function is impaired when compressed axons at one site cause the nerve to become especially susceptible to damage at another site.” Upton and McComas observed that a high percentage of patients with carpal, cubital, and radial tunnel syndromes also complained of unilateral shoulder, chest, and upper back pain. While the mechanisms involved in double crush syndromes are not fully understood, clinicians believe that nerves become sensitized and the brain and spinal cord undergo changes in how they modulate pain.5 While there are many peripheral nerve conditions, massage therapists often encounter thoracic outlet syndrome, radial nerve entrapment, cubital tunnel, and carpal tunnel syndromes.

An Example of Nerve Gliding and Tensioning
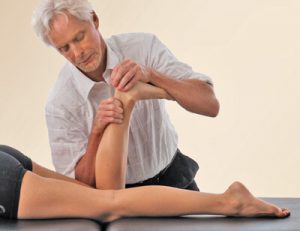
At the beginning of this blog I defined nerve gliding and tensioning. You’ll remember that nerve gliding, or flossing, is a manual technique where a therapist uses movement to pull a nerve back and forth along its path, similar to the action of dental floss in tooth care. Nerve tensioning elongates a nerve by placing it under gentle tensile force at both ends. When we apply these techniques during a massage session, a therapist passively moves some areas of the client’s body while the client actively moves others to elicit the proper glide or tension on a nerve.

01 Radial Nerve Gliding
For example, to perform nerve gliding on the radial nerve, as appropriate for radial nerve entrapment, you would move the client so that their right shoulder is slightly off the edge of the therapy table. Use your left leg to depress and brace the client’s shoulder. If the client reports pain when you depress and brace their shoulder, they likely have an issue proximally. You would address any proximal restrictions before you move forward with nerve mobilization.
Next, you would ask the client to curl their fingers around their thumb while you snake your right hand under their extended elbow and grasp their wrist, gently pulling it into internal rotation. Your left hand grasps the client’s closed fingers to flex the wrist and ulnar deviate it. Continue to flex and ulnar deviate the client’s wrist. At the same time, you extend the client’s elbow, maintaining pain-free motion, and then release the tension allowing the client’s elbow and wrist to return to a more neutral position. Check with the client to ensure this movement, which places the radial nerve under tension, doesn’t cause pain.

02 Sidebending and Rotation
Now, ask the client to left sideband and left rotate their head and then bring it back to neutral and continue to move into left sidebending and left rotation and then back to neutral at a slow and rhythmic pace. As the client’s head comes into the neutral position, you flex and ulnarly deviate the wrist while bringing the elbow into extension. As the client’s head left sidebends and rotates, you bring the elbow, wrist, and hand into a neutral position. The client is pulling the nerve to the left, and you are pulling the nerve to the right. Continue in this way at least five times to glide and floss the nerve.

03 Radial Nerve Tensioning
Next, as the client left side bends and left rotates their head, you flex and ulnar deviate the wrist and bring the elbow into extension. Now the client is pulling the nerve left, and you are pulling the nerve right to tension the nerve. Remember, mobilization should not be painful. If it is painful, work more slowly and more gently.
An Integrated Approach to Neurodynamics
As with muscle and bone, nerves benefit from movement and suffer from sedentary lifestyles, fixed postures, and repetitive stress. Recent in-vitro studies showed that mechanical load applied to nerves initiates internal cell processes responsible for nerve myelination and homeostasis, including cell differentiation and neurite outgrowth.6 You’ll remember that myelin is an insulating layer that forms around nerves in the brain and spinal cord. The myelin sheath allows electrical impulses to transmit quickly along nerve cells. Neurite outgrowth refers to any projection from the cell body of a neuron. Outgrowths can be either an axon or a dendrite. These processes are essential for general nerve health and repair following injury.7
It’s also interesting to note that the clinical outcomes are disappointing when nerve tensioning is the only intervention used to address compression-related conditions.8 Conversely, good results occur when both nerve gliding and tensioning are used along with other manual methods to ensure peripheral nerves glide smoothly through healthy surrounding tissue.9,10

For this reason, Myoskeletal Alignment Techniques takes an integrated approach to neurodynamics. We don’t use nerve gliding and tensioning in isolation. Instead, we use various manual methods that stretch muscles and move joints, knowing that this will begin the process of mobilizing nerves. When any area is properly prepared, we move into nerve gliding and tensioning methods.
The positive outcomes from integrated approaches to nerve issues include reduced nerve adherence, increased neural vascularity, reduced nerve stiffness, and reduced pain.11 In addition, as the pain subsides, the brain down-regulates sympathetic firing, and muscles stop splinting related joints restoring pain-free functional movement.
If these techniques are a good fit for your bodywork career, I encourage you to seek training in nerve mobilization. Nerve mobilization is advanced work requiring proficiency in anatomy, palpation, and client communication.
References
- Shacklock, M. Clinical Neurodynamics: A New System of Neuromusculoskeletal Treatment. Elsevier Health Sciences, 2005.
- Sung, J., Sikora-Klak, J., Adachi SY., et al. Decoupled epineurial and axonal deformation in mouse median and ulnar nerves. Muscle Nerve, Volume 59, Issue 5, 2019.
- Top, K.S., Boyd, B.S. Structure and Biomechanics of Peripheral Nerves: Nerve Responses to Physical Stresses and Implications for Physical Therapist Practice. Physical Therapy, Volume 86, Issue 1, 2006.
- Carp, S. Peripheral Nerve Injury: An Anatomical and Physiological Approach for Physical Therapy Intervention. F.A. Davis, 2015.
- Burke, Higgins, McClinton, Saunders, Valdata. Hand and Upper Extremity Rehabilitation: A Practical Guide, third edition. Elsevier, 2006.
- Carta, G., Gambarotta, G., Fornasari, B.E. et al. The neurodynamic treatment induces biological changes in sensory and motor neurons in vitro. Scientific Reports, 2021.
- Higgins, S., Lee, J.S., Ha, L., et al. Inducing neurite outgrowth by mechanical cell stretch. BioResources, 2013.
- Andrade, R.J., Freitas, S.R., Hug, F., et al. Chronic effects of muscle and nerve-directed stretching on nerve mechanics. Journal of Applied Physiology, Volume 129, Issue 5, 2020.
- Nee, R.J., Vicenzino, B., Jull, G.A. et al. Neural tissue management provides immediate clinically relevant benefits without harmful effects for patients with nerve-related neck and arm pain: a randomized trial. Journal of Physiotherapy, Volume 1, 2012.
- Fernandez-Carnero, J., Sierra-Silvestre, E., Beltran-Alacreu, H., et al. Neural tension techniques improves immediate conditioned pain modulation in patients with chronic neck pain: a randomized clinical trial. Pain Medicine, Volume 6, Issue 20, 2019.
On sale this week only!
Save 25% off the "Dalton Technique Treasures" eCourse
The “Dalton Technique Treasures” eLearning course is a compilation of some of Erik’s favorite Myoskeletal Alignment Techniques (MAT). Learn MAT techniques to assess and address specific sports injuries, structural misalignment, nervous system overload, and overuse conditions. ON SALE UNTIL July 29th! Get Lifetime Access: As in all our eLearning courses, you get easy access to the course online and there is no expiry date.