About 4,900 years ago, the Egyptians invented chairs, and the human spine has never been the same.1 Before humans had chairs, they squatted. Archeologists know this from markings on the bones of Neanderthal, paleolithic, and neolithic remains.2 For our ancestors, the deep squat was a comfortable position supported with minimal muscular activity and used to complete tasks low to the ground or to relax.3
People in Asian, African, Caribbean, and Latin American countries never abandoned the deep squat. If you’ve traveled to India or China, you’ve probably seen people tending their wares in the market in a relaxed squatting position. The cultural popularity of the deep resting squat may play a role in variations in the global pervasiveness of back pain. Estimates from the most recent Global Burden of Disease study found that Central Latin America, East Asia, the Caribbean, South Asia, and Sub-Saharan Africa had the lowest prevalence of low back pain. In contrast, Europe and North America had the highest prevalence of low back pain.4
All humans are born with the deep squat wired into their physiology. Watch children and you’ll see them maintain a deep sustained squat as they play. Toddlers have almost double the dorsiflexion of adults giving them the advantage of ankle mobility in a deep squat. However, most adults could comfortably squat if they practiced, and regular squatting could counter many of the muscle imbalances that come from our modern seated lifestyles.

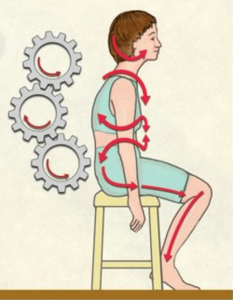
The Vicious Cycle of Lower Crossed Syndrome
Imagine that you spend most days hunched in front of a computer. Soon, your gluteal and abdominal muscles weaken. As a result, your body must recruit other muscles to facilitate normal activities of daily life. Recruitment causes overuse and hypertonicity, sometimes initiating a vicious cycle where the abdominal and gluteal muscles continue to deteriorate functionally.
Czechoslovakian neurologist and professor of manual medicine Vladimir Janda introduced the theory of crossed syndromes in 1979.5 While Janda’s muscle imbalance patterns may vary from client to client, many manual therapists have found them useful as a general assessment guide. In most clients presenting with a lower crossed syndrome, the abdominal and gluteal muscles are long and weak, while the hip flexors and lower back muscles are short and tight.
While treating the psoas is also important, releasing tension in the rectus femoris and retraining the body through deep squatting practices can help reciprocally strengthen weak inhibited muscles and will often break the cycle of lower crossed strain.

Rectus Femoris Treatment for Pelvic Bowl Rotational Patterns
In Myoskeletal Alignment Techniques, the Master Myoskeletal Therapist certification teaches advanced assessment and treatment for painful lumbopelvic disorders such as torsions, iliosacral up-slips, protective muscle spasms, and nerve impingement. There are many ways to address pelvic bowl rotational patterns. Today, we’ll use these rectus femoris techniques more generally to balance the pelvis.

Technique 01
With the client prone, grasp the client’s left medial thigh just above the knee with your right hand and flex the client’s knee to 90 degrees (shown in Image 2). Brace the client’s body with a firm counterforce by placing your left hand on the PSIS. Next, slowly lift the client’s leg into hip extension until you feel the first restrictive barrier or the client reports discomfort and hold. Ask the client to gently push their knee toward the therapy table to a count of five and relax. Lift the client’s leg until you feel the second restrictive barrier or the client reports discomfort and hold. Ask the client to gently push their knee toward the therapy table to a count of five and relax. Repeat this stretch on the right leg.

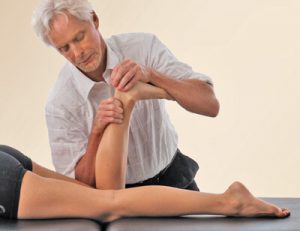
Technique 02
This technique helps balance the innominates by releasing the rectus femoris at the AIIS. With the client supine, stand on the client’s right side and place your right forearm softly above the client’s right knee. Drop into the rectus femoris and glide your forearm slowly toward the AIIS while communicating with the client about pressure and comfort. Repeat this technique three times and pause at the AIIS attachment site (shown in Image 3). While your right forearm pins the rectus attachments at the AIIS, your left hand internally and externally rotates the client’s leg. Repeat this technique on the left side.

Technique 03
Here, we learn a “shotgun” myoskeletal technique for addressing pelvic bowl rotation. A shotgun technique is a quick fix, in this case, for restoring balance and alignment in those presenting with an unleveling of the hips. To begin, ask the supine client to move to the edge of the therapy table and allow the right leg to drop off the table to extend the hip. Next, the client flexes their left knee and grasps it with both hands. Place your right hand on the client’s left knee and your left hand just above the client’s right knee. Apply gentle counterforce pressure with both hands. Next, ask the client to gently raise their right knee against your resistance to a count of five and relax. Now, apply a gentle counterforce by pushing the left hip into flexion and the right into extension and repeat three to five times. This is one of my favorite techniques for restoring balance and alignment to a distorted pelvic bowl.

Client Homework – Get to Know Squat
In a deep squat, the legs and feet are externally rotated and spaced about a shoulder’s width apart. The feet remain flat on the ground as the coccyx falls between the ankles, dropping the body’s weight down through the medial arches. The torso is straight. The chest lifts as the shoulders roll back and down. The low back rounds slightly. Relaxed thighs rest on the calves while the fingertips rest on the floor or the knees (Image 5).
This position strengthens typically weak, inhibited muscles, including the tibialis anterior, the peroneals, the gluteus maximus, and the hamstrings. As gravity pulls the buttocks down between the legs, the erectors, lumbar fascia, latissimus, and multifidus stretch. A significant stretch occurs in the rectus femoris muscles due to the knee-flexed position even with moderate trunk flexion.
You won’t recommend deep squatting to every client, as some have pre-existing ankle or knee conditions that present challenges or dangers. Similarly, we don’t want clients to force themselves into a deep squat. Instead, they should work towards a deep squat by holding onto the edge of a countertop to lower into position. Remind your clients to hinge at the hips and sit back as if they are sitting in a chair while keeping their chest up and their core engaged.
To come out of a squat, the client should push through their feet and activate their core as they return to a standing position. As their strength, balance, and flexibility improve, clients can drop into position without support, assume a deeper squat, and strive to perfect their form. Clients might spend ten minutes a day working on their squat or break up periods of sitting with deep squatting throughout the day.
Releasing a hypertonic rectus femoris and using the rectus femoris to level and align innominates has a profound balancing effect on the torsional forces arising through the pelvis in clients presenting with lower crossed syndromes. In addition, the daily practice of deep squatting can extend the outcomes clients experience during sessions. Soon inhibited muscles return to full function, breaking the strain cycle.
References
- Rybczynski, W. Now I Sit Me Down: From Klismos to Plastic Chair: A Natural History. Farrar, Straus and Giroux, 2017.
- Mays, S. The Archaeology of Human Bones, 3rd Routledge, 2021.
- Mays, S. The Archaeology of Human Bones, 3rd Routledge, 2021.
- Wu, A., March, L., Zheng, X. et al. Global low back pain prevalence and years lived with disability from 1990-2017: Estimates from the Global Burden of Disease Study 2017. Annals of Translational Medicine, Volume 8, Issue 6, 2020.
- Janda, V., Frank, C., Liebenson, C. Chapter 10, Evaluation of Muscular Imbalance. Rehabilitation of the Spine: A Practitioner’s Manual, 2nd Edition, edited by Craig Liebenson, Lippincott Williams & Wilkins, 2006.
On sale this week only!
Save 25% off the "Dalton Technique Treasures" eCourse
The “Dalton Technique Treasures” eLearning course is a compilation of some of Erik’s favorite Myoskeletal Alignment Techniques (MAT). Learn MAT techniques to assess and address specific sports injuries, structural misalignment, nervous system overload, and overuse conditions. ON SALE UNTIL July 29th! Get Lifetime Access: As in all our eLearning courses, you get easy access to the course online and there is no expiry date.