Sometimes clients don’t tell us the whole story. Such was the case with Mark, a 39-year-old competitive cyclist referred by a local chiropractor. During the history intake, he complained of sacroiliac joint pain that began after an accident while training for a cross-state cycling race. He and two other cyclists had collided on a tight turn, and Mark landed in a ditch on his right hip. After a quick Google search, he had self-diagnosed his condition as SI joint strain and insisted the chiropractor focus on that area. He was treated twice weekly for a month with little relief. When I asked Mark to place one finger on the most sensitive area, he simply said, “It hurts low down in the buttocks area.” When asked if he’d experienced similar symptoms before, he said he’d had the same pain a year earlier, but it had improved after he was advised by a fellow cyclist to change the slant on his bicycle seat.
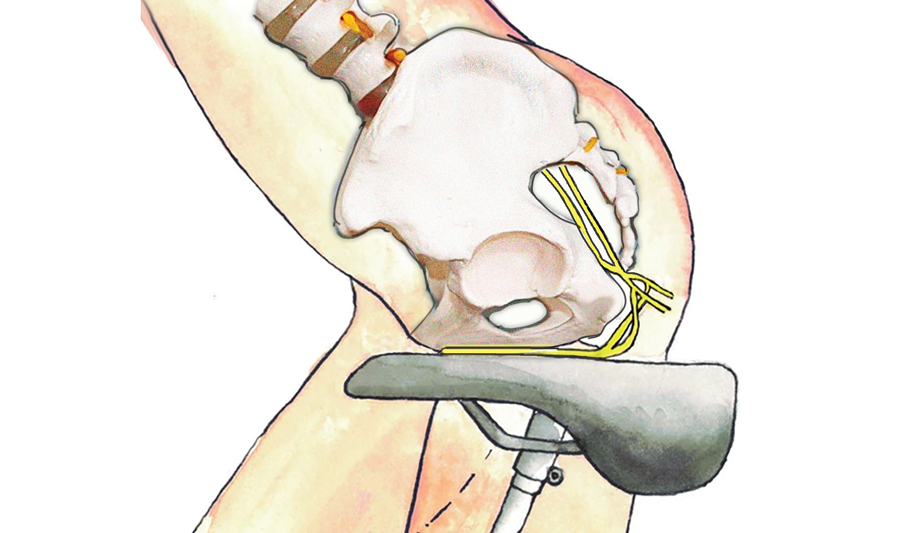
Mark was not wrong to think his pain may have resulted from trauma to the SI joint or its ligaments. However, once he disclosed he had previously suffered the same pain and that altering his saddle had helped, I immediately began to suspect pudendal nerve trauma. Pedaling while sitting on a slim, hard saddle and being constantly subjected to repetitive impacts can trigger extreme perineal pressure, which can directly or indirectly compress pudendal nerves (Image 1). An incorrectly positioned or improperly shaped bicycle seat may also result in tension or thickening of the sacrotuberous and sacrospinous ligaments, which can occlude branches of the pudendal nerve. Pain from this condition is reported in an astounding 50-to-91 percent of cyclists worldwide and simply results from spending too much time on a narrow bicycle seat.1
Pudendal Neuralgia
The name pudendal comes from the Latin word pudendum, meaning “parts to be ashamed of” — and clients may be reluctant to report any issues in this area. Pain from pudendal nerve trauma will typically refer into the groin area and in front of the rectum, slightly laterally. In men the pain often shoots into the posterior aspect of the testicles and penis, and in women the labia and lower vagina. The pain can feel deep and internal or more superficial like a burning, numbing, and prickly sensation. Pudendal nerve pain is usually more severe with sitting and relieved or improved by standing.
Although pudendal neuralgia is a relatively common long-distance cycling injury, most with this condition complain of painful sensations in their groin and scrotum — not in the hip. When I continued to question Mark about the exact location of his pain, he finally confided that sometimes he felt a stabbing pain in his testicles, but that his family doctor told him it was probably coming from an enlarged prostate gland
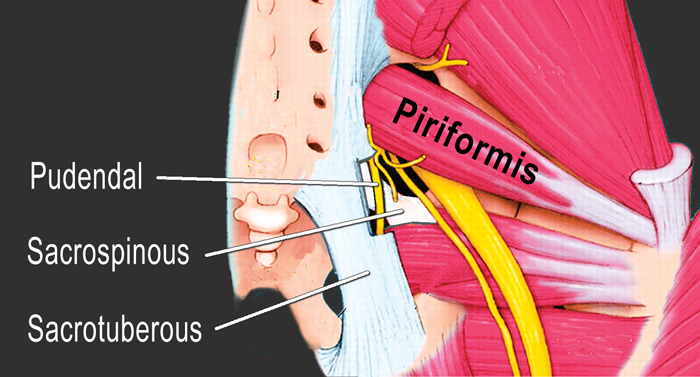
The pudendal nerve’s winding passageway through the pelvis makes it vulnerable to entrapment in several areas, but the two most common sites are between the piriformis and coccygeus muscles and between the sacrotuberous and sacrospinous ligaments (Image 2). Since there is no reliable pain provocation test, pinpointing pudendal neuralgia is an assessment of exclusion
To avoid confirmation bias on my part and assure Mark I was respecting his self-diagnosis, I ran him through a battery of SI joint orthopedic tests, all of which were negative.
Easing pudendal compression
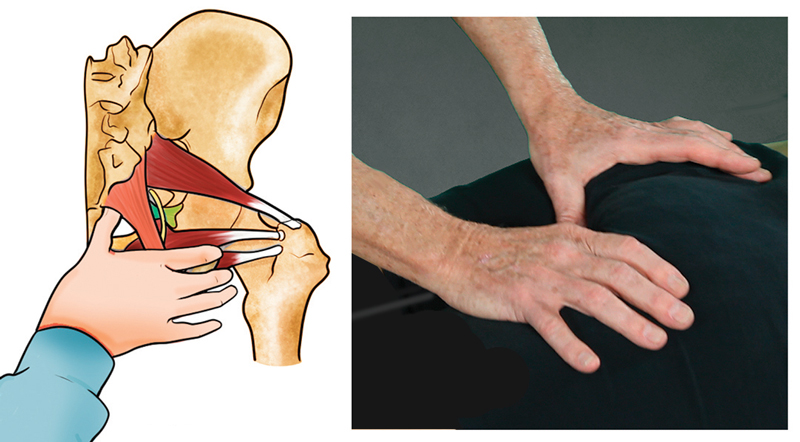
To help open the space between the sacrotuberous and sacrospinous ligaments on Mark’s right symptomatic side, I used my right thumb to hook under the contralateral sacrotuberous ligament just adjacent to the coccyx, then braced with my other thumb. Mark was then asked to begin a slow pelvic tilting motion while I gently but firmly pulled the ligaments off the pudendal nerve (Image 3). During the initial session, this maneuver elicited mild testicular pain, which did not occur in subsequent sessions.
In the image below you can see how I address Mark’s piriformis tightness. Muscle spasm in this area often squashes the pudendal nerve against the underlying coccygeus muscle, and indeed, the area was very congested. While working the external hip rotators, I had a feeling this may be the “main event” that had been triggering his pudendal nerve symptoms.
Following our fourth session, Mark began reporting less pain and was back to training for the big race. He was convinced the ligament and muscle work was responsible for the relief from his testicular pain. However, I credit some of the pain reduction to my physical therapist friend, who helped him retrofit his bike to better fit his body. Referrals are so important when it comes to improving performance and achieving overall wellness, and they certainly worked for Mark, who placed 11th in the cross-state race.

Summary
When dealing with suspected pudendal nerve pain, it’s important to remember that clients may be hesitant to discuss their condition due to the location of the referred pain. A careful intake and assessment can help them tell the whole story, drawing out the details needed to prepare an appropriate treatment plan.
References
- Leibovitch, I., & Mor, Y. (2005). The vicious cycling: bicycling related urogenital disorders. European Urology, 47(3), 277-287.
On sale this week only!
Save 25% off the Upper Body Course!
NEW! Enhanced video USB format!!!
Learn unique approaches to work with the shoulder girdle, arms, neck, and torso, this course will prepare you to relieve painful myoskeletal issues in the upper body. Through video demos and animation, you’ll learn to identify several compensatory movement patterns and their associated reflexogenic pain. With this understanding of where the true source of problems arise, you’ll be able to develop highly effective treatment protocols and deliver lasting results. This course provides you with the skills you need to confidently relieve pain issues in the upper body. (20 CE)
Bonus: When you order the Home Study version, get the eLearning course and and an additional 2CE Ethics eCourse for free!
Save 25% off the Upper Body Course this week only. Offer expires Sunday, March 1st. Click the button below for more information and to purchase the course for CE hours and a certificate of completion to display in your office.








