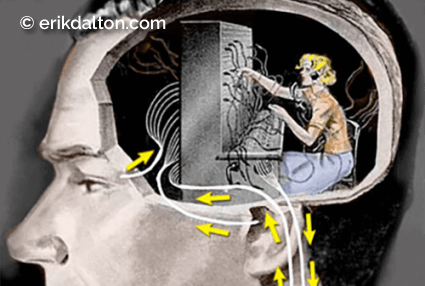
The head houses sensory organs called cranial teleceptors that connect us to the distant world. When floating comfortably atop the spine, cranial teleceptors reflexively orient head placement using light, sound, and gravitational sensory information. However, our brains are often unable to make sense of visual input without movement. The eyes must constantly move (saccades) for light to traverse across the retina, which allows the central nervous system (CNS) to construct visual images by comparing adjoining structures in the environment. Teleceptor function is compromised when the head is persistently maintained in an abnormal position. As spastic neck and jaw muscles inflict whole-body reflexive movement constraints, CNS “noise” heightens the body’s stress response.
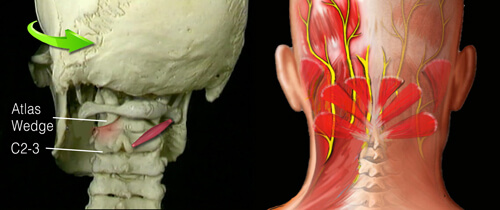
A catch-22 occurs when a poorly aligned body initiates HRR that trigger spasm and mechanically alter spinal joint movement. When hyperexcited joint and ligament mechanoreceptors initiate protective splinting, some muscles overwork and others are inhibited. This results in reduced mobility, excessive energy consumption, exhaustion, and, if the brain perceives threat, pain.
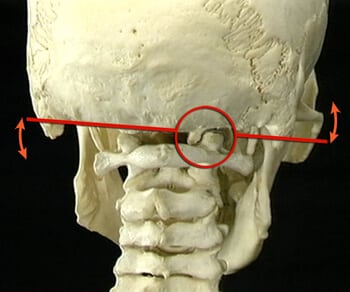
The occipitoatlantal (O-A) joint is the uppermost weight-bearing synovial joint in the body and is the final junction for adapting to asymmetry or dysfunction from below. Mechanically, the head teeters on the two condyloid joints (shaped like cupped palms tipped slightly medially) that make up the O-A joint (Image 1.). This design allows the head to nod back and forth and side to side. Since the O-A joint surrounds and attaches to the brain stem, which controls all basic body functions (including breathing and heartbeat), poor alignment may have widespread consequences.
O-A joint correction
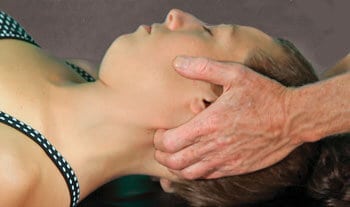
To relieve protective muscle guarding, begin by applying your favorite suboccipital technique such as the one shown in Image 3. Once the suboccipital hypertonicity has calmed, assess and correct O-A joint hypomobility by sliding the right hand under the supine client’s head while your left palm secures the forehead. Without lifting the client’s head, ask for a slow chin tuck toward the chest. As the head begins to flex on the neck, follow this movement with your right hand by softly pulling the back of the head superiorly, while the left hand gently pushes the forehead toward the eyebrows—imagine rolling a bowling ball using two hands (Image 4.). By applying a gentle two-second overpressure at the end of this chin tuck maneuver, you should be able to assess the ability of the occipital condyles to glide back on the atlas. If there is restriction to the chin tuck (i.e., a hard restrictive barrier), the O-A is unilaterally or bilaterally restricted.

To determine which side is stuck, simply right-sidebend the client’s head 20 degrees and repeat the chin tuck technique. If no resistance is encountered, test the opposite side by left-sidebending 20 degrees and rolling the head into flexion. If the chin does not want to approximate the chest with the head in this position, then the right occipital condyle is stuck anteriorly and is unable to glide back on the right atlas condyle. To free the soft tissues that are restraining joint motion, keep the client’s head in the same left-sidebent position and ask for a chin tuck while your hands follow with two seconds of gentle overpressure at the end range of flexion (stop if the client experiences any discomfort). Repeat three times and retest with the head in a neutral position.
Summary
Overall body balance is best achieved by leveling the head and tail during a single therapy session and retesting in subsequent visits. Try to include movement awareness dialog during your hands-on work and offer immediate feedback if you sense unnecessary effort or rigidity. Helping clients become aware of inefficient movement patterns is a learning process, not a procedure. Our bodies are shaped by how we use them, and habits determine use. It is the client’s underlying habits that need to change, and we can help. When confronted with pain and injury cases, rather than chasing the pain, first evaluate what the client may be doing to cause the problem, and help them learn how not to do it. Manual and movement therapy can then address abnormal neuromuscular righting reflexes that may be causing protective muscle guarding and accompanying joint dysfunction.
On sale this week only!
Save 25% off the Upper Body Course!
NEW! Enhanced video USB format!!!
Learn unique approaches to work with the shoulder girdle, arms, neck, and torso, this course will prepare you to relieve painful myoskeletal issues in the upper body. Through video demos and animation, you’ll learn to identify several compensatory movement patterns and their associated reflexogenic pain. With this understanding of where the true source of problems arise, you’ll be able to develop highly effective treatment protocols and deliver lasting results. This course provides you with the skills you need to confidently relieve pain issues in the upper body. (20 CE)
Bonus: When you order the Home Study version, get the eLearning course and and an additional 2CE Ethics eCourse for free!
Save 25% off the Upper Body Course this week only. Offer expires Sunday, March 1st. Click the button below for more information and to purchase the course for CE hours and a certificate of completion to display in your office.








