
The following is an excerpt from Erik Dalton’s book, Dynamic Body: Exploring Form Expanding Function, which features guest contributions from some of the leading thought leaders and practitioners in the massage profession.
Robert Schleip Ph.D., one of the leading figures in fascial research today, is the director of the Fascia Research Project, part of the division of neurophysiology at Ulm University in Germany. In this excerpt, he looks at two common mechanisms for how massage therapists stretch fascia and demonstrates how neither is sufficient to explain the effects of massage on fascia. The rest of the chapter can be read in the Dynamic Body textbook, available as part of the Dynamic Lower Body Home Study course or as a standalone purchase.
Thixotropy: The Gel-to-Sol Hypothesis
Piezoelectricity: Fascia as a Liquid Crystal
Fascial Plasticity: Traditional Explanations Insufficient
- either an extremely forceful stretch of three to eight percent fiber elongation, which will result in tissue tearing, inflammation, and other side effects that are usually seen as undesirable in a myofascial session. As an example, for an 18-millimeter-wide distal iliotibial band, such permanent elongation starts at 60 kilograms (kg). 14
- or it takes more than an hour (which can be taken at several intervals) with a less brutal one to 1.5 percent fiber elongation, if one wants to achieve permanent deformation without tearing and inflammation. 10,14
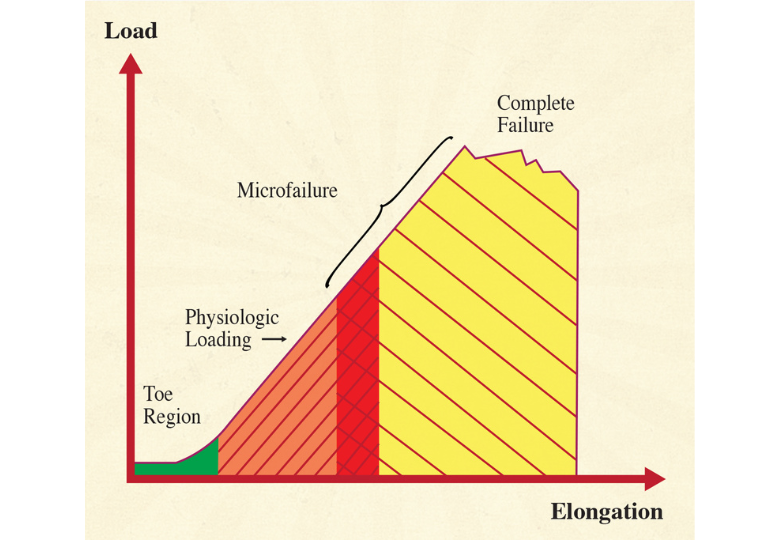
Figure 1. illustrates the typical relationships for short-term strain applications. Microfailure is seen as the breaking of some individual collagen fibers and some fiber bundles, resulting in a permanent (plastic) elongation of the tissue structure. This is usually followed by a cycle of tissue inflammation and repair. Based on measurements with different kinds of paraspinal tissues, A. Joseph Threlkeld, a professor of physical therapy, calculates that microfailure of most dense connective tissues occurs at around 224 to 1,136 N, which equals 24 to 115 kg.14 While high velocity thrust techniques might create forces within that range, it seems clear that the slower soft tissue manipulation techniques are hardly strong enough to create the described tissue response.
References
- Varela, F.J., & Frenk, S. (1987). The organ of form: towards a theory of biological shape. J Social Biol Struct, 10, 73-83.
- Barnes J.F. (1990). Myofascial Release: The Search for Excellence. Paoli, PA: Rehabilitation Services Inc.
- Cantu, R.I., & Grodin, A.J. (1992). Myofascial Manipu-lation: Theory and Clinical Application. Gaithersburg, MD: Aspen Publishers.
- Chaitow, L. (1980). Soft-Tissue Manipulation. Rochester, VT: Healing Arts Press.
- Paoletti, S. (1998). Les fascias – Role des tissues dans la mecanique humaine. Vannes cedex, France: Le Prisme.
- Rolf, I.P. (1977). Rolfing: The Integration of Human Structures. Santa Monica, CA: Dennis-Landman.
- Ward, R.C. (1993). Myofascial Release Concepts. In J.V. Basmajian and R.E. Nyberg (Eds.), Rational Manual Therapies. Baltimore, MD: Williams & Wilkins.
- Juhan, D. (1987). Job’s Body: A Handbook for Body-work. Barrytown, NY: Station Hill Press.
- Twomey, L., & Taylor, J. (1982). Flexion, creep, dysfunction and hysteresis in the lumbar vertebral column.Spine, 7(2), 116-122
- Currier, D.P., & Nelson, R.M. (1992). Dynamics of Human Biologic Tissues. Philadelphia, PA: F.A. Davis Company.
- Oschman, J.L. (2000). Energy Medicine. Edinburgh, United Kingdom: Churchill Livingstone.
- Athenstaedt, H. (1974). Pyroelectric and piezoelectric properties of vertebrates. Ann NY Acad Sci, 238, 68-110.
- Juhan, D. (1998). Job’s Body: A Handbook for Bodywork (3rd ed.). Barrytown, NY: Station Hill Press.
- Threlkeld, A.J. (1992). The Effects of Manual Therapy on Connective Tissue. Phys Ther, 72(12),893-901.
- Chaudhry, H., Schleip, R., Zhiming, J., Bukiet, B., Maney, M., & Findley, T. (2008). Three-Dimensional Mathematical Model for Deformation of Human Fasciae in Manual Therapy. J Am Osteopath Assoc,108(8), 379-390.
- Schleip, R. (1989). A new explanation of the effect of Rolfing. Rolf Lines, 15(1), 18-20.
- Still, A.T. (1899). Philosophy of Osteopathy. Kirksville, MO: Academy of Osteopathy.
- Kandel, E.R. (1995). Essentials of neural science and behavior. New York, NY: Appleton & Lange
On sale this week only!
Save 25% off the Upper Body Course!
NEW! Enhanced video USB format!!!
Learn unique approaches to work with the shoulder girdle, arms, neck, and torso, this course will prepare you to relieve painful myoskeletal issues in the upper body. Through video demos and animation, you’ll learn to identify several compensatory movement patterns and their associated reflexogenic pain. With this understanding of where the true source of problems arise, you’ll be able to develop highly effective treatment protocols and deliver lasting results. This course provides you with the skills you need to confidently relieve pain issues in the upper body. (20 CE)
Bonus: When you order the Home Study version, get the eLearning course and and an additional 2CE Ethics eCourse for free!
Save 25% off the Upper Body Course this week only. Offer expires Sunday, March 1st. Click the button below for more information and to purchase the course for CE hours and a certificate of completion to display in your office.








