The Myoskeletal Alignment Techniques program was developed as a tool to help relieve our nation’s neck/ back pain epidemic. By incorporating muscle-balancing techniques with joint-mobilization maneuvers, manual therapists learn to quickly identify and correct dysfunctional strain patterns before they become pain patterns.
This article is the first in a three-part series designed for massage therapists seeking more information about the reflexogenic relationship between muscles and joints. Combining muscle and joint modalities offers busy bodyworkers short-cuts that help shorten assessment/hands-on time, increase therapeutic efficiency; and provide clients with pain relief.
Part 2: Simplifying the Pain Puzzle
Part 3: Working Through the Dura Mater
What makes MAT special?
Well-documented theories explain how joints become fixated from myofascial stressors; yet relatively unknown in the massage therapy community is how joint dysfunction creates protective muscle spasm and dysfunctional strain patterns, such as forward head postures, slumped shoulders and scoliosis. This reflexogenic relationship between muscles and joints is the foundation of the Myoskeletal Alignment Technique and is considered not only uniquely different from traditional thinking, but possibly an important next step in addressing abnormal strain patterns caused by muscle/joint imbalances.
Massage therapists can now safely address all soft tissues, including ligaments, nerve dura, fasciae, discs and joint capsules, responsible for much of the pain previously blamed on muscles alone. Osteopathic methods, such as muscle energy, strain-counter strain and mechanical link, are also designed to relieve muscle/joint dysfunctions, but the MAT method complements today’s bodywork practices as it was specifically designed to fit a massage-therapy format.
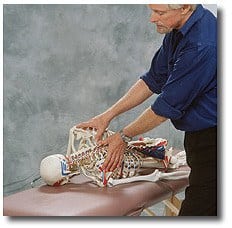
One distinguishing goal that establishes the MAT method apart from other techniques is its dependence on identification and correction of joint fixations. This is accomplished by systematically releasing deep spinal muscles, ligaments and fibrotic joint capsules that torsion and compress spinal joints. In some cases, a bodyworker may apply direct pressure to bones to release fibrotic muscles that create joint blockages, but the intent is always soft-tissue work.
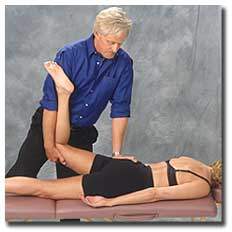
Assessment: Anterior Hip Capsule Adhesion
a. Following hip flexor work, the hip capsule is assessed and addressed by flexing the client’s left knee and locking her foot with the therapist’s right shoulder.
b. The palm of the therapist’s left hand braces just inferior to the ischial tuberosity so a counter-force between the two hands can be established as the left leg is lifted into extension.
c. The client is asked to lightly push her knee toward the table while the therapist resists this effort to a count of five.
d. The client relaxes and the therapist slowly pulls with his right hand while resisting with his left hand.
e. The therapist should feel joint play in the capsule and iliofemoral ligament.
f. Repeat the technique to loosen the joint capsule and iliofemoral ligament.
Note: This technique is contraindicated for clients with hip replacements or joint pathology.
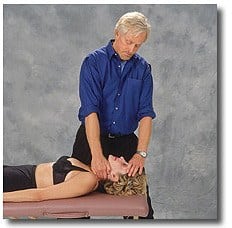
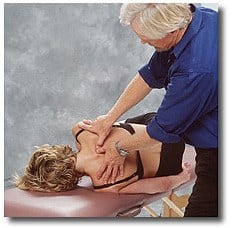
Assessment: Deep Spinal Rotator Muscles
a. The therapist secures the client’s forehead with his left hand and reaches under with a flat palm so his fingers can grip deep rotators in the cervical lamina groove.
b. The client inhales to a count of five while attempting to gently turn her head left against the therapist’s resistance.
c. As the left spinal rotator muscles fire, the therapist searches for and releases fibrotic knots in the lamina groove. The client relaxes. Repeat on the opposite side as necessary.
Posture’s Role
Most manual therapists today agree that no therapeutic approach to neck/back pain is complete unless body posture is generally improved. Whatever the root of the client’s condition, special attention must be dedicated to posture-especially the correct positioning of the pelvis. Many therapists complain that postural assessments are often too complex, too time-consuming, too clumsy-in a typical massage setting with the client draped.
The MAT method lessens assessment anxiety with an efficient five-minute hands-on evaluation that quickly identifies gross body asymmetries, such as pelvic tilts, short legs, sacroiliac dysfunctions, scoliosis, facet restrictions and hip-capsule adhesions. MAT also incorporates Vladimir Janda, M.D.’s upper-and-lower crossed visual assessment method for easy recognition of muscle-imbalance patterns that cause neck and low-back pain. Combining these hands-on and visual assessment techniques allows the therapist to immediately tell which muscles are tight and pulling unevenly on the body’s bony framework, and which weak muscles are permitting the asymmetry. Janda’s muscle-imbalance research has gifted bodywork practitioners with a remarkably useful model for explaining how predictable muscle imbalances cause predictable faulty postural patterns, such as slumped shoulders, forward heads, swaybacks and dowager’s hump. (Hands on procedures using Janda’s formula are detailed in Part II of this series.)
Ultimately, for long-lasting relief of chronic neck/back pain, the MAT system works to achieve these goals:
- balancing the head on the neck
- balancing the neck on the shoulders
- balancing the shoulder girdle on the rib cage
- balancing the pelvis on the femurs
- restoring pain-free movement
Recent studies have confirmed a noticeable reduction in noxious neural input entering the spinal cord and brain when the postural goals listed above are met. In 1979, biomechanical researcher J. Gordon Zink, D.O., coined the term “common compensatory patterns” to describe routinely found postural patterns in the neuromyofascial-skeletal system. His studies were the first to validate how structure and function play a dual role in posturally initiated pain syndromes. Eventually, he concluded that postural muscle stress leads to chronic, recurrent central nervous system irritation initiated by sensory receptors, such as mechanoreceptors, nociceptors and chemoreceptors.
Postural muscles are structurally designed to resist fatigue and function in the presence of prolonged gravitational exposure. If their capacity to resist stress is lost, the postural muscles become irritable, tight and shortened. Fortunately, as balance and function are re-established in distorted myofascial structures, hyperactivity in agitated joint and muscle receptors rapidly dissipates. Zink’s conclusion leads to the underpinnings of the client’s outcome: less sympathetic muscle spasm, less limbic system activation, less stress-and less pain.
How Muscles Reveal Joint Dysfunction
During a presentation to the American Back Association in the early 1990s, Phillip Greenman, D.O., unlocked the door to a brave new world of possibilities for massage therapists searching for new ways to locate and address muscle spasm when he said, “In the presence of vertebral dysfunction, palpable fourth-layer muscle fibrosis will always be found.” What a simplified way for therapists to identify areas of joint dysfunction and spasm.
Professional bodyworkers’ sensitive fingers and thumbs often dig through the bulky erector spinae muscles into underlying fourth-layer spinal muscles (multifidus, rotatores, levator costalis and intertransversarii). Frequently palpated are small, hard and sometimes tender knots in these deep-tissue structures. Until now, the reason for their continued presence has remained a mystery; but, with the advent of new, more sophisticated electromyographic equipment, researchers are beginning to understand how joint misalignment promotes hypertonicity in these little spinal-rotator muscles.
The MAT system has adopted Greenman’s practical and efficient method for identifying joint dysfunction by teaching students how to palpate for fibrotic knots in the deep spinal-rotator muscles. Truly remarkable is the power these little fourth-layer transversospinalis muscles can generate. They easily pack enough punch to lock spinal joints open or closed with their strong torsional forces. Clients complaining of cricks in the neck are frequently suffering from unilateral hypertonicity and shortness in the intertransversarii muscles. Running from transverse process to transverse process, when fibrotic, these little devils like to side-bend the neck, locking the facets closed on the ipsilateral side or open on the contralateral side.
The intertransversarii are one group of muscles that should never be addressed with direct finger-pressure in the cervical region, to avoid injuring surrounding neural and vascular structures. But a therapist trained in MAT bypasses this problem by using bones as levers to release these tight little side-benders.
By gently applying specific directional pressure to the neck’s bony articular pillars, the therapist waits for a Golgi tendon organ release in the intertransversarii.
Intertransversarii Muscles
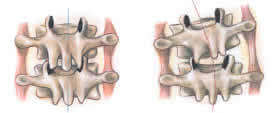
Facet joints stuck closed on right during flexion efforts

Because fourth-layer muscles, such as the intertransversarii, are among our phylogenetically oldest intrinsic muscles, they must be assessed and released in all neck routines to ensure proper cervical alignment. Applying Greenman’s assessment approach allows massage therapists to quickly locate areas of joint dysfunction simply by scanning the spinal groove and searching for lumpy fourth-layer tissue.
Hypertonic knots found in deep transversospinalis muscles always indicate joint dysfunction, but exactly what does this information reveal about the condition of the joint fixation? Nothing! It doesn’t tell whether the joint is locked open or closed-only that there is dysfunction at that level. Fortunately, that is all the information needed at this time using the MAT assessment system. To determine if the joint is locked open or closed, the therapist simply flexes and extends the involved area while palpating the fibrotic knot. If the bony knot pushes back when flexion is introduced, the joint is not opening on that side. If the knot pushes back during extension movements, the joint is not closing on the opposite side, forcing the vertebra to rotate back against the therapist’s palpating fingers.
Keeping It Simple
The MAT system intentionally simplifies correction of joint-related tissues by systematically releasing lumpy, fibrotic fourth-layer muscles, ligaments and joint capsules with the client in flexed and extended positions. Specific directional pressure is then applied to the bony knots until the lamina groove is smooth. Ida Rolf, Ph.D., included groove work at the end of each of her very popular 10-session Rolfing ® series. With the client seated and slowly flexing forward, she would frequently shout orders to “go for a smooth groove” as the students elbowed their way down the lamina groove. (Obviously, she was in tune with the enormous therapeutic value of proper alignment in this area.)
The advanced MAT program includes post-isometric relaxation techniques combined with specific breathing maneuvers to help clear stubborn knots that distort the groove. Simple motion tests alert the therapist to the type of fixation (i.e., whether the joint is stuck open or closed). Once the therapist determines the exact type of dysfunction present, joint play and capsular flexibility can usually be restored using the MAT method-but not always. In some cases the joint has undergone adherent cartilage degradation and facet “nipping” (microtrauma). The resultant facet degeneration causes a true adhesive joint problem. Obviously, this presents a more serious condition than tight muscles restricting joint movement. Working in close cooperation with chiropractors and manipulative osteopaths, prompt referrals should be made along with details describing the specific location of the dysfunction.
Myoskeletal therapy delves deep into body structures, but the intent is still low-force soft-tissue work and should feel exactly like a good deep-tissue session. Bones are addressed as soft-tissue structures in the MAT system, with pressure often applied directly to transverse processes. But bones are only used as levers to release hard-to-access fourth-layer muscles and fibrotic joint capsules. Joints should never be taken into a non-physiologic range of motion, as this would be outside the scope of practice of massage therapists.
Receptors: Backbone of the Myoskeletal System
Input to the central nervous system relies on receptors for detecting sensory stimuli, such as pain, touch, sound, light, heat and cold. Classified according to their actions, these receptors describe their specific duties, such as mechanoreceptors, nociceptors, chemoreceptors, thermoreceptors and electromagnetic receptors. Their primary task is to change sensory stimuli into action potential so information is continually fed to the central nervous system concerning the person’s overall body environment. Many researchers believe our bodies are receptor-driven and that these receptors are the key factor in interacting with our environment. Most massage therapists are familiar with sensory receptors, such as Golgi tendon organs and muscle spindles, but new studies substantiate the presence of other types of receptors located in frequently forgotten soft tissues of the body.
Historically, the medical and manual therapy communities have generally regarded soft tissues, such as ligaments, fasciae, joint capsules and discs, as only mechanical structures and not neurological mediators. But recent technical advances in nerve-staining techniques have revealed the presence of neural elements in all these spine-related tissues. In 1995 Hanging Jiang, Ph.D., and his associates documented the presence of mechanoreceptors and nociceptors in human supraspinal and interspinal ligaments by following 10 patients before and after spinal decompression surgery. His complex and lengthy research ultimately supported earlier scientist’ findings that ligaments, discs and fasciae are integral parts of an intricate neurological feedback loop beautifully designed to protect and stabilize the spine.
Scientists are now finding that ligaments, intervertebral discs and facet capsules are blessed with a rich supply of mechanoreceptors and free nerve endings called nociceptors that alert the brain to undue stress in joint-related tissues. Nociceptors and chemoreceptors are activated when nerve fibers are depolarized by high mechanical stresses in the joint capsule or by exposure to inflammatory chemical agents, such as histamines, prostaglandins, kinins, potassium ions and lactic acid.
When nociceptors fire in response to actual tissue damage, they quickly become major generators of both myofascial- and spinal-pain syndromes. Long-term central nervous system agitation from angry nociceptors causes the brain to twist and torque the body in an effort at pain avoidance. Regrettably, the brain has the ability to memorize these aberrant postural patterns and relearn them as normal. When the dysfunctional pattern persists long after the painful stimulus has been removed, scientists refer to the condition as neuroplasticity, reflex entrainment or spinal learning. Clients whose bodies remain distorted long after the pain has subsided present a therapeutic challenge to today’s bodyworker. Fortunately, home retraining exercises that incorporate a variety of movement patterns often help break this neurological hard-wiring problem.
Sensory Receptors and Massage Therapy
Previously found only in animal specimens, articular receptors, such as mechanoreceptors and nociceptors, have only recently been identified in human spinal tissues. The impact of these recent discoveries holds widespread significance for massage-therapy procedures. For example, it now appears that much of the spasticity and pain reported by clients might originate not only from toxic muscles and trigger points, but from irritated mechanoreceptors, nociceptors and chemoreceptors in misaligned, injured or restricted joint soft tissues. Armed with this new information, therapists can address their clients’ needs more effectively by applying special massage maneuvers to restricted joint capsules, spinal ligaments and deep transversospinalis muscles to desensitize unhappy joint receptors.
The MAT approach to improving function through structural balance always begins with conventional muscle/ fascial balancing routines. But once the therapist manages to restore optimum myofascial flexibility and symmetry, the intent changes. Focus is then directed toward calming joint receptors simply by locating and releasing restricted facet joint capsules. Robert Gillett, D.C., found that only 40 neutons of force is required to co-activate all these mechanically sensitive joint receptors.
(Footnote 1)
A Sample MAT Session
Facet opening at T4-5
- In this example, the client’s right T4-5 joint won’t open as she flexes forward, causing the T4 vertebrae to rotate right.
- To begin the correction, the client is positioned on the left side lying/flexed posture with the left arm behind her back. This position encourages the right rotated T4-5 joint to attempt left rotation, which is the direction it needs to go in order to open.
- The client is then instructed to grasp the side of the therapy table with her right hand, tuck her chin, take a deep breath to the count of five and gently pull up against the isometric resistance of the therapy table. This action fires the short spinal-rotator muscles, causing the dysfunctional T4 vertebra to push back right against the unyielding pressure of the therapist’s thumbs.
- As the thumbs gently resist this effort during client exhalation, slow, sustained thumb pressure begins to move the T4 transverse process in an anterior/superior direction to open the stuck facets.
Facet opening at T4-5
- Using soft fingers or thumb pads, the therapist slowly digs through the deep fourth-layer spinal rotator muscles, searching for joint adhesions.
- Co-activation of hyperactive receptors at T4-5 is accomplished by applying mild, sustained thumb pressure to the misaligned vertebral transverse process of T4.
- The question is: Why is the therapist mobilizing T4 rather than T5?
The process is repeated until the therapist feels a softening in the surrounding paravertebral tissues and the bony knot disappears into the contour of the lamina.
It is important to remember that although the therapist’s thumbs are pushing on bone, the intent is only to release the adhesive joint capsule and hypertonic rotator muscles that are preventing the T4-5 facet joints from opening. Application of sustained pressure to the transverse process during this technique has two very beneficial effects: As the client pulls up on the table with the therapist’s thumbs resisting her effort, a powerful Golgi tendon relaxation response is activated through the transverse process to the rotatores, multifidi, intertransversarii and levator costalis muscles; as the client exhales, a post-isometric relaxation response is automatically elicited in these tight spinal-rotator muscles, allowing deeper thumb penetration and easier release of the fibrotic soft tissues causing the joint blockage.
If the joint opens as it should, the therapist will feel an instantaneous release in the neighboring soft tissues and a palpable reduction in protective muscle guarding. However, if little change is felt, the therapist must retest to see if the fixation released completely. If the joint appears to be opening on both sides as it should but muscle spasm is still evident, then the rib adjoining the vertebral dysfunction at T4-5 has become stuck in external rotation and must be addressed using the same general procedure as above. Referred to as a dual-fixation, this vertebra/rib condition falls among the most painful, long-lasting and overlooked of all client complaints.
Why Muscles Spasm
The massage-and-bodywork community is well aware of the many ways toxic muscles progress from soreness into painful spasm, contractures and trigger points. Sustained isometric muscle contraction from trauma, tension and poor posture are obvious culprits.. Relatively less recognized, however, is the important role joint dysfunction plays in the development of muscle spasm and related myofascial pain syndromes. Muscles are the body’s primary movers and must respond quickly to all changes coming from neural structures. When tight muscles pull unevenly on spinal joints, the joint’s axis of rotation is disrupted and the center of gravity changes. Sensory nerve receptors located in spinal joint capsules, ligaments, discs and deep transversospinalis muscles become aggravated from prolonged joint misalignment.
Particularly unhappy are mechanoreceptors embedded in overstretched capsules or in the part of the joint bearing excessive weight. Range-of-motion restriction from adhesive tissue build-up in the capsule causes eventual loss of joint play.
- Sensitive joint receptors react by flooding the spinal cord and brain with noxious afferent messages that set off warning bells of spinal instability or possible tissue damage
- To prevent further insult to the painful area, the cerebellum and gray matter react by locking up all back and neck muscles with protective muscle spasm, as described earlier
- When over stimulated muscle, ligament, disc and joint-capsule receptors join forces and suddenly discharge on axon terminals in the neuronal pool, subthreshold stimuli quickly escalate into full-blown central nervous system attacks
- This consolidated surge of noxious stimuli leads to jamming of neurologic pathways. In his book Palpation Skills, Leon Chaitow, D.O., refers to this insidious condition as “cross talk.” (Footnote 2)
To complicate the situation, excessive interactive neural build-up from the effects of cross-talk layer the body with stubborn chronic spasm. The longer these powerful asymmetric myofascial forces are allowed to twist and compress the body’s bony framework, the more noxious stimuli is generated. This marks the beginning of a devastating, self-perpetuating pain/spasm/pain cycle that massage therapists battle each working day. Amazingly, researchers still do not know if impaired function of a muscle(s) is the primary cause of joint dysfunction or if the reverse is true.
Regardless of whether muscle or joint receptors initiate these painful cycles, bodyworkers usually call upon conventional muscle/ fascial techniques to deal with the painful spasm, fibrotic knots and trigger points. Myofascial techniques work extremely well in situations where spasm and myofascial shortening have not significantly altered joint alignment; however, in many cases the pain has long passed the sore muscle stage into a condition referred to as microtrauma. Basically, microtrauma is a slow-developing degenerative joint condition commonly caused by overuse, underuse or abuse. This silent villain cleverly disguises itself as a deep muscle ache. Clients who continually complain of chronic “between-the-shoulder-blade pain” often inaccurately assume this persistent irritation to be a muscle problem. But the pain and suffering usually results from inflamed rib-heads and intervertebral joints agitated by prolonged joint misalignment.
New Therapeutic Massage Tools
Muscle-related joint therapy offers today’s bodyworkers added therapeutic tools to aid clients suffering recurring, mysterious and aggravating pain or posture problems. Massage therapists who routinely see musculoskeletal pain problems will relish the synergy of both power and practicality in these new reflexogenic muscle/ joint routines. Because traditional massage techniques alone solve much of the neck/ back pain puzzle, always begin each therapy session using conventional myofascial balancing routines. Tight, hypertonic muscles are lengthened using myofascial release, assisted stretching and receptor co-activating techniques, and weak, inhibited muscles are tonified with fast-paced, spindle-stimulating maneuvers. Once myofascial balance is restored, remaining joint-related dysfunctions can be more easily assessed and corrected.
Today’s manual therapist will soon discover the added therapeutic benefits of integrating joint capsule, spinal ligament and intervertebral disc routines into their existing practices. Some massage and bodywork schools in the United States are already introducing students to the fascinating world of spinal biomechanics through complementary therapies, such as muscle energy, orthobionomy, medical massage and mechanical link.
Many teachers in the current, constantly evolving bodywork community understand how application of deep-tissue techniques to the body’s intrinsic muscles alters alignment in the skeletal system. What affects one always affects the other. Therefore, it is helpful to seek a basic understanding of joint mechanics and the laws of spinal motion before addressing clients with random deep-tissue techniques.
A safe therapist is a knowledgeable, holistic therapist. Simply put, the more the therapist knows, the safer the therapist becomes. Initially, an introduction to the concept of combining muscle-joint modalities might appear complex. But soon the therapist will recognize the marvels of muscle-joint relationships. Through hands-on training and continued studies, an exciting new world of therapeutic possibilities opens up, as the trained bodyworker wholeheartedly experiences the reflexogenic relationship between muscles and joints-a welcome addition to the therapist’s toolbox of touch.
References
- Gillette, R.G. Journal of Manual Medicine 3:1, 1987.
- Chaitow, L.. Palpation Skills, Churchill Livingstone, New York, 1998.
Please note: These articles and the accompanying photographs are not a substitute for hands-on training. Readers are urged to seek training and/or to self-assess to make sure they have sufficient education and experience to understand the information presented here and to safely perform the techniques described.
On sale this week only!
Save 25% off the Upper Body Course!
NEW! Enhanced video USB format!!!
Learn unique approaches to work with the shoulder girdle, arms, neck, and torso, this course will prepare you to relieve painful myoskeletal issues in the upper body. Through video demos and animation, you’ll learn to identify several compensatory movement patterns and their associated reflexogenic pain. With this understanding of where the true source of problems arise, you’ll be able to develop highly effective treatment protocols and deliver lasting results. This course provides you with the skills you need to confidently relieve pain issues in the upper body. (20 CE)
Bonus: When you order the Home Study version, get the eLearning course and and an additional 2CE Ethics eCourse for free!
Save 25% off the Upper Body Course this week only. Offer expires Sunday, March 1st. Click the button below for more information and to purchase the course for CE hours and a certificate of completion to display in your office.








