Manipulating nerve receptors in joints can be very effective in relieving spasms and pain.
Most massage therapists know that the tiny nerve terminals called receptors, such as Golgi tendon organs (GTOs) and muscle spindles, cause muscles to contract and relax. New biomedical studies reveal the presence of other types of receptors located in frequently overlooked soft tissues of the body, such as the neck. This knowledge can serve as a clue to understanding how we interact with our environment and enjoy balanced movement, postural awareness and internal homeostasis.
Soft-tissue specialists should have a basic understanding of these fascinating receptors and their relationship to neck pain and posture. Also, this knowledge might help spawn new approaches to helping clients in need.
Receptors Defined
Receptors detect sensory stimuli such as touch, pain, heat, sound, light, and cold, and communicate this information to the central nervous system. An efficient neurological feedback system then informs the brain of changes in the person’s overall body environment.
Sensory receptors of greatest concern to massage therapists can be classified according to the mechanism of their actions. Besides GTOs and muscle spindles, these include mechanoreceptors, thermoreceptors, nociceptors, electromagnetic receptors, and chemoreceptors.
Historically, medical and manual therapists have regarded soft tissues as forming embryonically from the mesoderm. For instance, ligaments, fasciae, intervertebral disks and joint capsules have been cataloged as supportive, or mechanical, structures, not as neurologic mediators. However, recent advances in nerve-staining techniques reveal the presence of tiny nerve receptors embedded in all myoskeletal tissues. These ongoing studies lead neuroscientists to conclude that ligaments, fasciae, discs and joint capsules:
- Participate in normal neuromuscular reflexes, such as active balancing of the spine when walking and standing (proprioception).
- Warn the brain of pain-producing stimuli that also may be causing tissue damage.
- Inform the brain of stresses and strains from tension, trauma and poor posture.
When something goes haywire, the neck becomes painful, resulting in devastating and widespread effects.
Logically, there should be neck techniques to turn off, or coactivate, hyperexcited receptors that tighten myofascial tissues and distort posture. Likewise, there should be techniques to turn on, or activate, weak, inhibited tissues that fail to support the spine and cause neck pain. A handful are explained here.
Chronic Pain
In a remarkable feat of engineering, the neck’s sturdy but flexible system of muscles, ligaments and fascia provides support for the 10-pound head, while allowing flexion, extension, rotation and sidebending in countless combinations. When something goes haywire, the neck becomes painful, resulting in devastating and widespread effects.
Myofascial Release®, deep-tissue, triggerpoint and assisted-stretching techniques effectively lengthen shortened or hypertonic muscles, while strengthening exercises address the weak, inhibited tissues.
Traditional massage therapy maneuvers successfully coactivate cutaneous receptors in the skin and superficial fascia, thus promoting a temporary relaxation response. As the tissues elongate, blood, oxygen and vital nutrients replenish the cells, as waste products are carried away. However, for stubborn chronic-pain conditions, articular receptors must also be coactivated by adding enhancers to the session.
It is now known that chronic muscle imbalance patterns develop from abnormal afferent information, due to poor posture, trauma, joint blockage, emotional stressors and habitual movement patterns. Massage therapists need to understand this reflexogenic influence that joints have on muscles that tug on cervical structures, and lead to long-term head, neck and scapular pain.

The following three modalities focus on receptors to help clients suffering from chronic neck, thoracic and brachial pain:
- Activators: Application of fast-paced, muscle-stimulating maneuvers using fingers, fists and forearms to activate (turn on) weak muscles.
- Coactivators: Application of sustained pressure to tendon GTOs, spinal ligaments and joint capsule mechanoreceptors to calm hypertonicity and to restore elasticity.
- Enhancers: Combining active and passive client movements while deep GTO pressure is applied to tendons, ligaments and joint capsules.
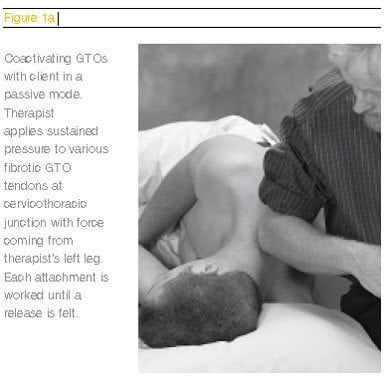
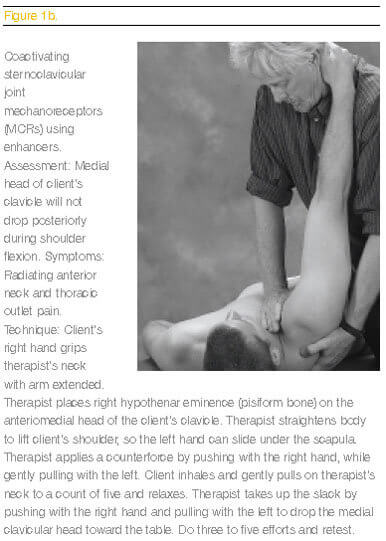
Through the combination of active and passive client movements, with the therapist holding sustained tendon, ligament or capsular pressure, joint receptor hyperactivity is normalized and joint-play is restored. Figures 1a and 1b below demonstrate examples of passive and active myoskeletal maneuvers for turning off hyperactivity in muscles and joint receptors.
Weak Muscles
When the brain senses weaknesses in an area, it quickly recruits surrounding muscles to splint the area, so that further insults to delicate neural structures housed in the spine are prevented. There is enormous therapeutic value in the muscle spindle. It is considered the third-most-complex sensory organ after vision and hearing. Fortunately, there are practical hands-on techniques that can effectively stimulate spindle fibers to turn on weak muscles.
To confront muscle and joint imbalances and begin blocking chronic pain cycles, the therapist can approach the dysfunction in a couple of ways: Begin the muscle balancing session by lengthening the short, neurologically facilitated muscles that pull unevenly on the spine; or, tonify the weak, inhibited muscles that permit the asymmetry.
The muscle spindle has a built-in mechanism called the dynamic gamma motoneuron (DGM) system. This is designed to measure small, quick fluctuations in a muscle’s length. By applying specific fast-paced, spindle-stimulating maneuvers with the fists, fingers or forearms, the therapist can elicit a tonifying stretch reflex in the muscle.This is a very valuable tool for waking up weak muscles.
Typically, weak inhibited muscles, such as the lower shoulder stabilizers (lower trapezius and rhomboid major), become neurologically activated when specific spindle-stimulating techniques manually create contractibility in these muscles. Strengthening the lower shoulder stabilizer and posterior rotator cuff muscles helps to conquer the slumped, shouldered posture caused by powerful pectorals. As the brain senses this newfound stability in the shoulder girdle, it neurologically causes protective muscles in the scapular stabilizers to release; this, in turn, reciprocally decreases pectoral tightness.
 These scapular-balancing routines can be successful when the muscle(s) to be activated are put on the stretch, and, when the fast paced manual pressure is forceful enough to cause simultaneous movement of both the weakened muscle’s origin and its insertion (see Figure 2 below). If these two criteria are not met, the DGM system may refuse to tonify the neurologically weakened muscles.
These scapular-balancing routines can be successful when the muscle(s) to be activated are put on the stretch, and, when the fast paced manual pressure is forceful enough to cause simultaneous movement of both the weakened muscle’s origin and its insertion (see Figure 2 below). If these two criteria are not met, the DGM system may refuse to tonify the neurologically weakened muscles.
It is an astonishing experience to feel the tight pectorals reciprocally release as the lower-shoulder stabilizer muscles are turned on. When the brain senses that the spine is better supported, its neurological muscle guarding in the deeper structures will be released.
Tight Muscles

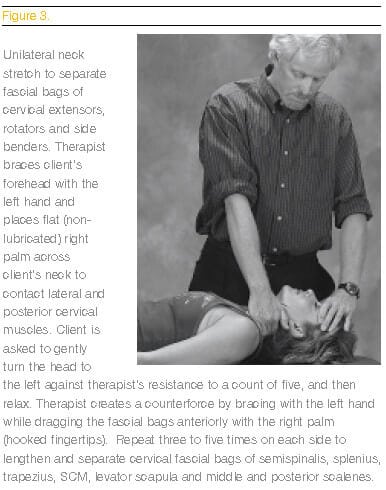
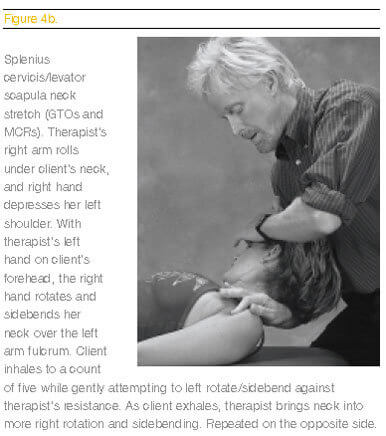
Traditional techniques that range from Myofascial Release, trigger point therapy and assisted stretching, to various deep-tissue modalities can be used to palpate and lengthen tight, short muscles. In Figure 3, the therapist begins with myofascial softening strokes—using flat, relaxed palms and hooked fingertips—to separate the fascial bags between the trapezius, levator, splenius, posterior scalenes and semispinalis muscles. Such prep work is suggested before proceeding to deeper GTO, mechanoreceptor (MCR) and assisted stretching routines, such as those shown in Figures 4a and 4b below.
Sustained pressure to tendon attachments, while the muscle is either actively contracting or on the stretch, coactivates Golgi stretch receptors. This increases muscle length. Such deep GTO pressure resets the muscle’s length and also inhibits or relaxes its synergistic stabilizers (muscles that perform a similar action). Most importantly, through reciprocal innervation, GTO pressure facilitates its antagonist.
Researchers do not know the primary cause of joint dysfunction However, a reflexogenic relationship exists between muscles and joints.
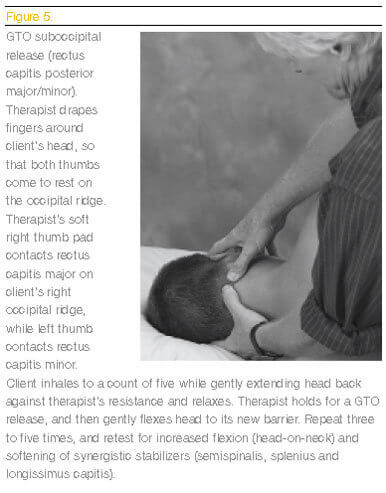
As seen in Figure 5, the therapist applies a suboccipital release to rectus capitis posterior major and minor, causing all the synergistic stabilizer muscles that also attach along the occipital ridge (splenius capitis, semispinalis capitis, longissimus capitis) to become neurologically relaxed. Meanwhile, the deep-neck flexor antagonists (longus capitis) are strengthened through reciprocal innervation.
Unfortunately, the act of releasing the suboccipitals only works on the neurological component. It will not eliminate fibrosis or contractures in their synergistic stabilizers. Only finger and thumb techniques that systematically dig out thick fibrosis and chronic contractures will restore flexibility to muscles, ligaments and joint capsules in this area.
Joint Dysfunction

Joint dysfunction plays an important role in the development of muscle spasm and related myofascial pain syndromes. Researchers do not know if impaired muscle function is the primary cause of joint dysfunction, or if the reverse holds true. However, a reflexogenic relationship exists between muscles and joints. Long-term chronic neck pain seems to be primarily caused by facet-sticking from swollen, adherent or degraded articular cartilages in the synovial facet joints.A second major contributor to recurrent neck pain is bone-spurring in the little nonsynovial structures that guide the nerve roots away from the spine (uncovertebral joints of Luschka).
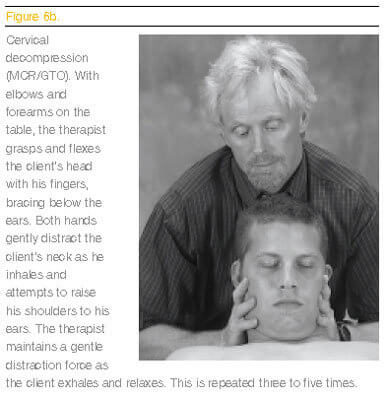
As tension, trauma, poor posture and gravitational exposure flatten the discs, the resultant hypermobility begins to pull the posterior longitudinal ligament away from the bony margins. Internal bone pressure fills the cracks with spurs. Along the way, osteophytes scratch the nerve dura, triggering the sinuvertebral nerve to sympathetically cause spasm. Fortunately, these chronic-pain generators can be lessened by applying specific soft-tissue decompression maneuvers to facilitate rehydration of flattened intervertebral discs, thus relieving dural drag. (See Figures 6a below, and 6b on the opposite page.)
As the body’s primary movers, muscles must respond quickly to all changes directed by neural structures. Prolonged sitting, while holding a telephone with one shoulder, often causes muscles, such as the levator scapula and splenius cervicis, to tighten and pull the neck to one side. As the facet joints jam shut, the joint’s axis of rotation is disrupted and the neck’s center of gravity is altered.The group of crooked joint capsules and restraining ligaments are overstretched on the convex side, while the discs and facet cartilages are unmercifully squashed on the concave side.
Sensitive mechanoreceptors embedded in the capsules, ligaments and discs respond to such excessive mechanical loading. After prolonged compression from motion-restricted joints, they begin flooding the spinal cord with noxious afferent messages. As sustained torsional forces in the neck dehydrate the synovial fluid, cartilages degrade, inflammatory waste products accumulate, and then the chemoreceptors become sympathetically agitated. With both mechanoreceptors and chemoreceptors involved, the nociceptors communicate spinal instability, pain and possible tissue damage to the brain.
Nociceptors are nonadapting. Pain refuses to subside until the joint’s alignment is improved, or the pain-producing stimulus is removed. As the nociceptors continue to warn the brain, the cerebellum reacts by locking the neck with protective muscle spasm to prevent further insult to the sensitive spinal structures.
Of course, the resulting pain-spasm-pain cycle compounds the situation.The therapist often will feel the tight spasm opposite the side where the client reports pain. This is the brain’s attempt to pull the neck away from the squashed discs and facets on the tight side. Now the neck must endure bilateral compressive forces in a pain-spasm-pain cycle. The visual consequence is a forward head posture. (See Figures 7a and 7b.)
Forward-Head Pain
Bilateral compression of neural or vascular structures causes the brain to selectively recruit specific muscles. Particularly hard hit with spasm are the SCMs, suboccipitals and anterior scalenes. As these muscle groups neurologically hypercontract, the neck moves forward on the thorax beginning with C7 on T1, C6 on C7, C5 on C6, and so on. The heavy head is finally forced to cock back into hyperextension on the subtle neck through the OA joint to help the eyes achieve a level. Since the upper cervical complex (occiput, atlas and axis) works as a team, distortion at the craniocervical junction can trigger tonic neck reflexes that travel down intersegmental pathways. This can cause weird pain or scoliotic patterns through the trunk and into the pelvis.
To alleviate cervical compression resulting from forward head postures, the therapist can systematically release muscles, ligaments and joint capsules using receptor techniques, such as those shown in Figures 8a, 8b and 8c on Page 86. As each successive vertebra slides forward on its inferior neighbor, the cervical curve straightens.This causes the gravitational weight to transfer from the intervertebral discs to the posterior facet joints.
Facet joints are possibly the most innervated structures in the spine.They are designed to support only 15 to 20 percent of the weight of the head. Thus, prolonged compression results in excessive mechanoreceptive, chemoreceptive and nociceptive activity. Increased weight transferred from the vertebral bodies to the agitated posterior facet joint cartilages continues to send noxious stimuli to the cerebellum, stimulating another layer of protective spasm.
This, in turn, triggers the SCM, suboccipital and anterior scalene muscles to pull the head even farther forward on the saggital plane. This sets the stage for a catch-22-like painspasm- pain cycle that ends in dowager’s hump, osteoporotic cracking and disc degeneration.
Soft-tissue techniques to release the hypercontracted muscles may be helpful in the short run. However, for long-term relief, precise hands-on receptor techniques must address the mechanoreceptors, chemoreceptors and nociceptors in spinal ligaments, joint capsules and compressed discs.
Finally, vital cervical tissues, such as the ligamentum nuchae, can be effectively treated.This ligament is a stabilizing structure for muscle and fascial attachments in the neck and head. Researchers suspect that neurofibers may actually penetrate the foramen magnum along with rectus capitis posterior minor. The infiltrating fibers in these two structures possibly evolved to help secure the dural membrane during the variety of movements essential for upright posture.
Injury or strain to this extremely important ligament sets off a blast of mechanoreceptive and chemoreceptive activity, making it a major source of chronic head and neck pain. Figure 9 illustrates a powerful coactivating mechanoreceptor release of the ligamentum nuchae at the inion, the lowest bump in the occipital midline.
Receptor Glossary
Abbreviations:
- GTO: Golgi tendon organ
- MCR: Mechanoreceptor
- NOC: Nociceptor
- CMR: Chemoreceptor
- SPD: Spindle
Definitions
- Golgi tendon organs: Measure tension buildup in muscles. GTOs are found in a series within muscle fibers, and are stimulated by both passive and active muscular contraction. When tendon tension becomes extreme, the inhibitory effect from the GTO can be so great that there is a sudden relaxation of the entire muscle under stretch.
- Mechanoreceptors: All three types of mechanoreceptors are activated by mechanical pressure from distortions in facet joint capsules, ligaments, discs and fascia. Mechanoreceptors, by nature, respond to loads (stretching or compression) placed on the tissues in which they lie.
- Nociceptors: Commonly regarded as pain generators, these receptors warn the brain of the possibility of tissue injury. Under normal circumstances, the nociceptive system is silent, which means it is not receiving enough sensory stimuli to elicit a painful sensation. But when adequately stimulated, nociceptors fire continually in a nonadapting way until the stimulus is removed. There are three types of stimuli that excite nociceptors: mechanical, thermal and chemical. Prolonged nociceptive irritation can cause clients’ bodies to twist and distort in an effort at pain avoidance. Unfortunately, these distorted postures can be relearned as normal, leading to conditions called neuroplasticity, reflex entrainment or spinal learning.
- Chemoreceptors: Receptors that become activated by a buildup of chemical substances. Hyperexcited chemoreceptors react by flooding the spinal cord with noxious afferent stimuli. Toxic waste byproducts from prolonged tissue damage cause inflammation. Fibrin deposition in muscles, ligaments, joint capsules and fasciae occurs as the inflammation dries.
- Muscle spindles: The muscle spindle, the third-most-complex sensory organ, after the eyes and ears, is the receptor responsible for the stretch reflex or myotatic reflex arc. Muscle spindles’ parallel arrangement within muscle fibers allows them to respond to passive muscle stretch, but they cease to discharge if the muscle contracts isotonically.
Conclusion
Researchers have determined that structures, such as ligaments, fasciae, joint capsules and intervertebral discs, are innervated and can participate in normal neuromuscular reflexes, some of which result in pain. Myoskeletal therapy engages a joint’s receptor system, using enhancers and activators. Enhancers can be any micro or macro movement performed by the client that puts an activating force through the neuromyoskeletal system to affect cutaneous, as well as articular, receptors. This technique may be applied for the relief of chronic neck pain.
On sale this week only!
Save 25% off the Upper Body Course!
NEW! Enhanced video USB format!!!
Learn unique approaches to work with the shoulder girdle, arms, neck, and torso, this course will prepare you to relieve painful myoskeletal issues in the upper body. Through video demos and animation, you’ll learn to identify several compensatory movement patterns and their associated reflexogenic pain. With this understanding of where the true source of problems arise, you’ll be able to develop highly effective treatment protocols and deliver lasting results. This course provides you with the skills you need to confidently relieve pain issues in the upper body. (20 CE)
Bonus: When you order the Home Study version, get the eLearning course and and an additional 2CE Ethics eCourse for free!
Save 25% off the Upper Body Course this week only. Offer expires Sunday, March 1st. Click the button below for more information and to purchase the course for CE hours and a certificate of completion to display in your office.