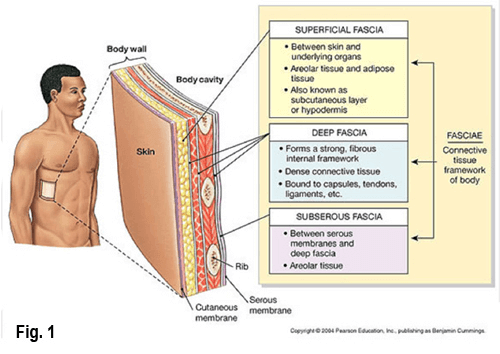
There’s a saying in orthopedics that “motion is lotion for joints,” but what about muscles, fascia, and neural structures? Aging causes us to produce less synovial fluid for joint lubrication, and hyaluronic acid for musculofascial gliding (Fig. 1). Consequently, each day our bodies “dry up” a bit, get a little shorter, and hurt more if the brain feels threatened by this structural collapse.
Living structures are perfectly adapted to work with maximal efficiency and low levels of energy. Sadly, our clients often present as noisy machines, which waste a lot of energy. But, motion is lotion and some believe that nothing stirs up the juice like good bodywork and corrective exercise. The burning question is: “can manual and movement therapists actually enhance lubrication to stuck fascial layers, adhesive joint capsules, and injured ligaments and, if so, how?”

Hyaluronic acid (HA) is present in every tissue of the human body. It is most concentrated in the synovial fluid, which bathes the joints, but also appears at the junction between the deep fascia and the muscle layers (Fig. 2). At the 2012 Vancouver Fascia Research Congress, I attended a full-day workshop conducted by Drs. Antonio and Carla Stecco. Their research generally focuses on how inadequate hyaluronic acid due to lack of movement, postural stress, or tissue injury and inflammation, may be responsible for fascial adhesions. 1
In this hands-on presentation, participants were taught a fascial manipulation technique (localized frictioning to areas of palpable rigidity), designed to generate heat. The intended effect alters chemical reactions within tissues causing a reduction in secretion of inflammatory cytokines (small proteins important in cell signaling). A clinical study conducted by the Stecco group found that it takes an average of 3.4 minutes of deep friction for a perceptible change to occur in rigid tissues. 2
In a fully functioning body, fascial layers secrete HA which allows smooth gliding between fascia and neighboring muscles. But, tissue trauma, overuse, and resultant inflammation can cause overproduction of HA, leading to molecular fragmentation and degradation. In time, the granulated particles form a sticky, dehydrated gel, which may decrease fluidity, resulting in a binding or “gluing” of myofascial layers.
As the brain orders the muscles to fire, it is speculated that altered viscoelasticity affects the fascia’s ability to elongate. This change in viscosity causes an increase in the production of HA, which has anti-inflammatory properties. The ability to manually promote better drainage of inflammatory waste products is one possible explanation for the changes therapists feel when performing soft tissue or joint mobilization work. Additionally, any reduction in the chemical irritation of fascial and joint sensory receptors may cause a reduction in pain, and a renewed freedom of movement.
Whether the release we feel is from the ‘gel-to-sol’ hyaluronic acid transformation or a neural explanation such as fascial mechanoreceptors, practitioners must first hone their palpation skills to differentiate quality, range and end-feel of various soft tissues including ligaments and joint capsules.
In summary, it is thought that tissue trauma due to overuse or injury may cause fascial deformation and dysfunction, but further studies are needed.
References
- Roman M, Chaudhry H, Bukiet B, Stecco A, Findley TW. Mathematical analysis of the flow of hyaluronic acid around fascia during manual therapy motions, J Am Osteopath Assoc. 2013
- Borgini E, Stecco A, Day JA, Stecco C, How much time is required to modify a fascial fibrosis? J Bodyw Mov ther. 2010
On sale this week only!
Save 25% off the Upper Body Course!
NEW! Enhanced video USB format!!!
Learn unique approaches to work with the shoulder girdle, arms, neck, and torso, this course will prepare you to relieve painful myoskeletal issues in the upper body. Through video demos and animation, you’ll learn to identify several compensatory movement patterns and their associated reflexogenic pain. With this understanding of where the true source of problems arise, you’ll be able to develop highly effective treatment protocols and deliver lasting results. This course provides you with the skills you need to confidently relieve pain issues in the upper body. (20 CE)
Bonus: When you order the Home Study version, get the eLearning course and and an additional 2CE Ethics eCourse for free!
Save 25% off the Upper Body Course this week only. Offer expires Sunday, March 1st. Click the button below for more information and to purchase the course for CE hours and a certificate of completion to display in your office.








