Getting to the bottom of buttock pain...
The buttock has been assigned more syndromes than any other bodily region. This is due to the biomechanical complexity of the sciatic nerve and the tremendous torsional forces traversing the pelvis and lumbar spine during daily activities. Piriformis syndrome, gemelli-obturator internus syndrome, ischial tunnel syndrome, and greater trochanteric pain syndrome are but a few of the names used to describe symptoms associated with tendinopathies and sciatic-nerve entrapment sites in the buttocks. Special orthopedic tests may help rule out possible offenders, and a comprehensive intake aids in detecting biopsychosocial factors that may be contributing to the client’s pain. However, the problem I often encounter when assessing buttocks pain is symptom overlap, which can make pinpointing the exact location difficult and unreliable. So, in this blog, I’ll use the umbrella term deep gluteal syndrome (DGS) to describe generalized sciatic-related buttock pain. I’ll also outline a few techniques I’ve found helpful in freeing up musculofascial tissues that may be possible perpetrators.
Sciatic nerve mobility and flexibility
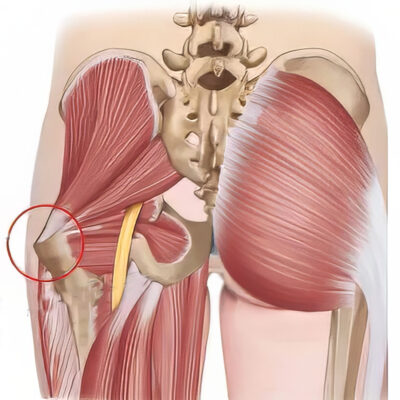
Covered on top by the gluteus maximus muscle, the sciatic nerve travels between the ischial tuberosity and the greater trochanter of the femur on its way to innervate the legs and feet (Image 1.). Researchers have found the sciatic nerve has 28 millimeters of excursion during hip flexion, and under normal patterns of joint movement, it’s flexible enough to stretch and slide to give way during moderate strain or compression.1 However, trauma, injuries, or repetitive motion activities can cause tethering, inflammation, and — if the brain perceives threat — pain. Below is a routine I’ve found helpful in relieving symptoms for two of the most common buttock conditions.
Easing the hip’s external rotators
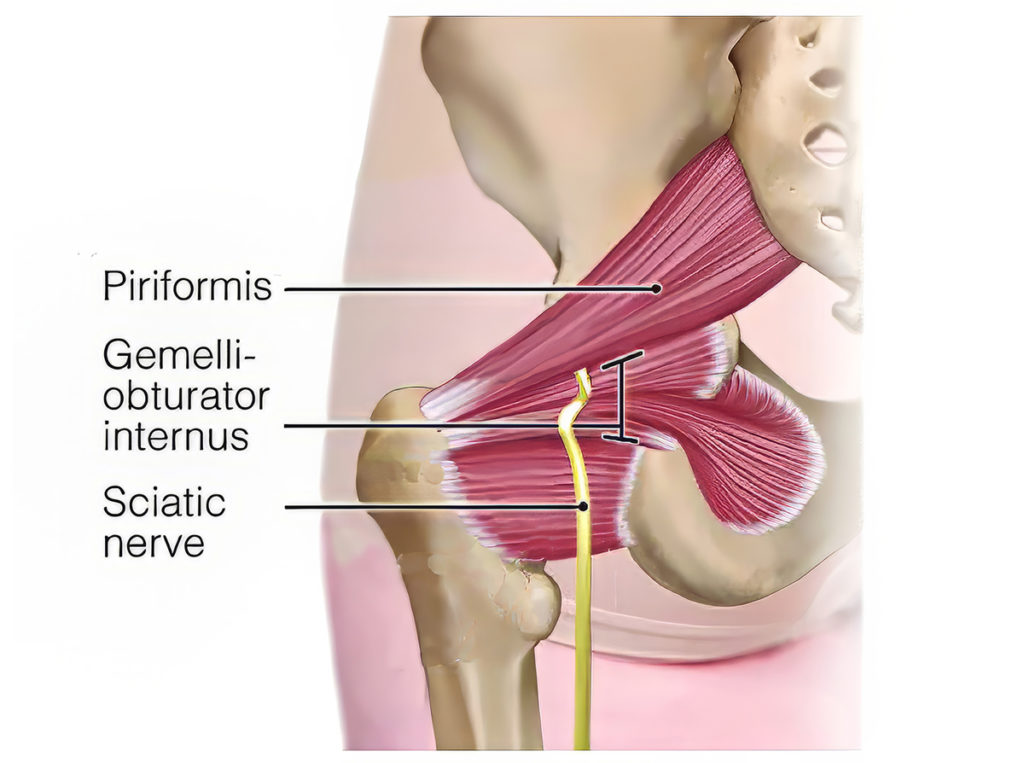
I typically begin by addressing three of the “deep six” external hip rotators as they insert at the greater trochanter. Note in Image 2. how the sciatic nerve can become kinked between the piriformis and gemelli-obturator internus muscles. To help soften fibrotic bands that may be compressing the sciatic nerve, my right forearm contacts and fascially hooks the piriformis, gemelli, and obturator internus tendons at the posterior border of the greater trochanter while my left hand braces the client’s thorax. A counterforce occurs as my right forearm gently drags the tendons inferiorly while my left hand resists (Image 3.). The client is asked to begin slow anterior and posterior pelvic tilting as I resist this motion.
Note: None of these techniques are performed on those with hip replacements or diagnosed hip and lumbar spine pathology.

Mistaken identity
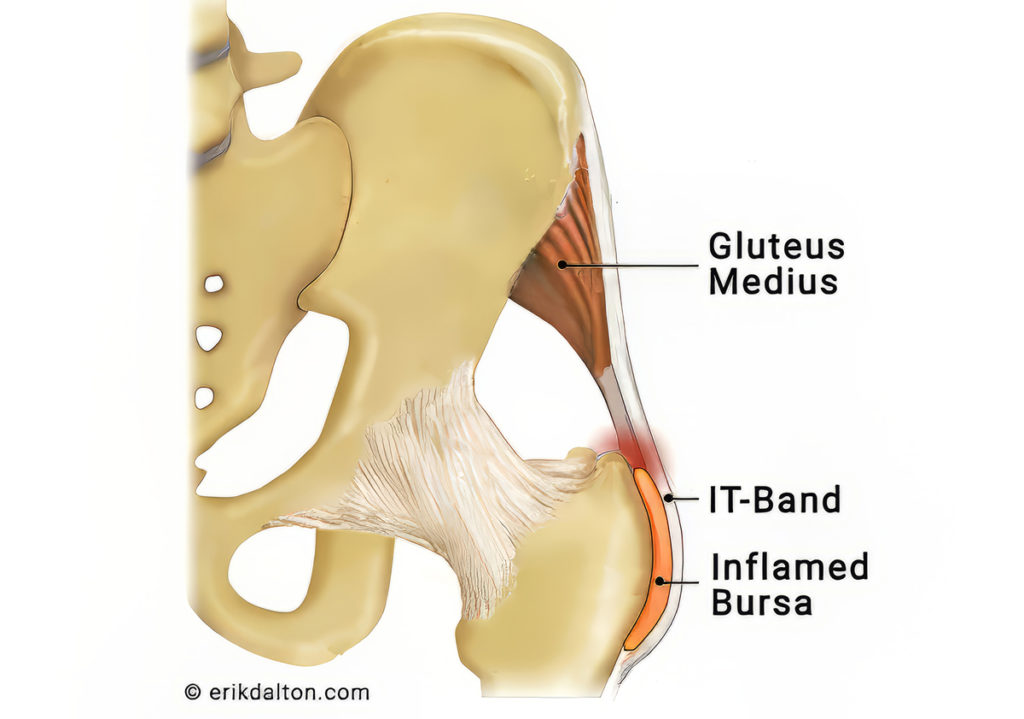
Greater trochanteric pain syndrome is a disorder of the gluteus medius and minimus tendons — gluteal tendinopathy — but is often mistaken for DGS. In some clients, there’s accompanying irritation in nearby structures, including the greater trochanteric bursa and IT band (Image 4.). Since the bursa and IT band are affected by the same mechanisms of overuse or injury, treatment aims to minimize irritating load and ease compression in neighboring tissues. Recall the lateral fibers of gluteus medius are hip abductors and the anterior fibers are internal hip rotators. Therefore, in Image 5. I begin by slightly adducting and externally rotating the client’s thigh. With his knee flexed 90 degrees, a graded exposure pin-and-stretch maneuver is performed by bringing the client’s thigh into more external rotation while resisting the motion with my soft left palm. As the first restrictive barrier is reached, the client is asked to gently push his leg toward me to a count of five and relax. I repeat the maneuver by increasing external hip rotation with my right hand and resisting with my left to the next pain-free restrictive barrier.
After repeating three times, I position the client face up and apply another more direct “shotgun” stretch to the gluteal tendons and lateral hip rotators. (Image 6.)


Summary
Since words like “pinched” or “entrapment” can evoke fear, I find it less threatening to tell the client with DGS the sciatic nerve may be getting irritated on its path from the spine through the buttock and into the thigh. If the client asks for more details, I may refer to their pain as “nerve-related buttock pain,” then specify which nerve is most likely involved. Anatomical models are great teaching tools for nerve compression and tendinopathy syndromes as long as the description is informative and non-threatening.
References
1. Martin, H.D., Reddy, M., & Gómez-Hoyos, J. (2015). Deep gluteal syndrome. Journal of Hip Preservation Surgery, 2(2), 99-107.
On sale this week only!
Save 25% off the Upper Body Course!
NEW! Enhanced video USB format!!!
Learn unique approaches to work with the shoulder girdle, arms, neck, and torso, this course will prepare you to relieve painful myoskeletal issues in the upper body. Through video demos and animation, you’ll learn to identify several compensatory movement patterns and their associated reflexogenic pain. With this understanding of where the true source of problems arise, you’ll be able to develop highly effective treatment protocols and deliver lasting results. This course provides you with the skills you need to confidently relieve pain issues in the upper body. (20 CE)
Bonus: When you order the Home Study version, get the eLearning course and and an additional 2CE Ethics eCourse for free!
Save 25% off the Upper Body Course this week only. Offer expires Sunday, March 1st. Click the button below for more information and to purchase the course for CE hours and a certificate of completion to display in your office.








