Part one: Sacrificing Complexity of Movement for Stability
Many injuries in America today result from on-the-job muscle/joint strain and overuse syndromes. Working in a technologically driven society has caused an explosive and expensive increase in work-related costs, with injuries occurring to categories of workers previously considered low risk for anything more serious than the occasional paper-cut.
Often seen as a structurally subtle body segment, the neck is burdened with the highly difficult task of supporting the human head. Because of the tension, trauma and poor posture inherent in today’s workplace, it is no surprise that head-on-neck and neck-on-thorax imbalances serve as some of the most common pain generators driving people into our bodywork practices.
This two-part series is excerpted from the author’s new textbook, Advanced Myoskeletal Techniques. This issue’s segment investigates the causes, conditions and corrections associated with one of the most painful of all postural faults: forward-head postures.
The battle against gravity
Muscles are designed to glide independently neighboring myofascial tissues as the central nervous system orchestrates a complex array of specified movements. When observing professional gymnasts at work, one immediately recognizes the astonishing quality, variety and complexity of their coordinated movement patterns. Conversely, the elderly foot-shuffler appears to have body areas frozen in time. Sadly, years of tension, trauma and poor posture—combined with gravitational exposure—force the human body to sacrifice complexity of movement for stability.
Today, more than ever, people are inclined to sit for hours in isometrically contracted postures without adequate physical activity. When muscles contract, fuel is burned and waste products accumulate. In time, these chemical irritants alter the muscles’ resting length, causing enveloping fascial bags to lose their natural suppleness. Prolonged sitting leads to slumping, as people spend countless hours tied to work terminals, home computers, school desks and television sets. As the heavy head slowly drops forward and down, the scapulae externally rotate and protract, increasing thoracic kyphosis and flattening of lumbar lordosis.
Exhausted from battling gravity, intrinsic cervical extensor muscles such as semispinalis, longissimus, the suboccipitals and multifidus become toxic from oxygen deprivation. Extrinsic (phasic) muscles (trapezius, rhomboids, posterior rotator cuff, etc.) prefer burning glucose for fuel but the deep intrinsic support muscles require more oxygen. When tension, trauma and faulty posture reduce the amount of delivered to intrinsic postural muscles, fatigue sets in, causing the gravitational load to shift to the extrinsics.
Extrinsic muscles are dynamic and designed to provide quick bursts of energy Since phasics contain a greater number of fast-twitch fibers, they do not respond well to sustained compressional loading and quickly give out and the energy-depleted intrinsic muscles are once again made to bear the load. This decompensation cycle marks the beginning of a domino effect that structurally manifests as: reduced flexibility; loss of range of motion; and an unattractive, forward-head, slumped-shouldered posture.
The gluing process
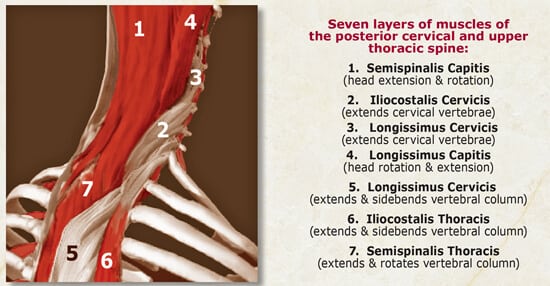
The seven deepest myofascial layers traversing the C7-T1 junction are particularly vulnerable to sustained isometric contraction from forward-head postures (Figure 1). With time, the slick lubricating fluid designed to provide smooth gliding of individual fascial sheaths dehydrates, thickens and becomes adhesive. The result: fascial adhesions, myospasm and muscle contractures. Living in a healthy body with pain-free range of motion requires that every upper quadrant muscle maintain its own independent yet communal contribution during head-and-neck movements. When “sticky” fascial layers bond, specialized (efficient) muscle movement is lost. The semispinalis, splenius, longissimus and trapezius fasciae are often guilty of clinging and dragging on neighboring muscles.
Myofascial restrictions not only waste precious energy but also reduce flexibility and range of motion. An exaggerated example of this condition is often seen in persons forced to turn their entire trunk to look to the side. This population usually presents with protracted shoulders and forward-drawn heads evolved from years of slumped sitting, repetitive movement patterns, trauma, and limbic system (emotional) stressors. Names such as fibromyalgia and chronic fatigue syndrome are often assigned to describe these achy, energy-deficient bodies.
Technically speaking, a positive test for a forward-head posture requires that the zygomatic arch (under the eye) be more than three centimeters forward of the sternoclavicular joint. Researchers generally agree that for every inch the head shifts forward in the sagittal plane, the neck’s extensor muscles are required to isometrically restrain (against gravitational force) not only the head’s weight, but also an extra 10 pounds for each inch of forward head migration. Therefore, a 12-pound head that moves three inches forward of the thorax forces the cervical extensor muscles to support a 42-pound head against the incredibly formidable influence of gravity.
The neurology of forward heads
The human body’s bony framework and supporting soft tissues are densely populated with proprioceptive and pain-sensing sensory receptors that serve as the frontline of awareness. Faulty posture, micro- and macro-trauma, gravitational stress and resultant inflammation cause a breakdown of the smooth self-regulating function of these receptors. Soon the person begins to experience painful spasmodic episodes, as caustic waste products such as histamines, bradykinins and lactic acid collect in the tightened, nutrient-depleted muscle bellies. Prolonged toxic buildup stimulates sensitive chemoreceptors that flood the spinal cord and brain with noxious messages setting off neurologic inflammatory responses.
Sustained isometric muscle contraction not only excites inflammation-sensitive chemoreceptors, but also specialized mechanoreceptors designed to monitor excessive stretching or compression of joint capsules, ligaments, discs, fascia and spinal rotator muscles. As chemoreceptors and mechanoreceptors bombard the spinal cord with perpetual streams of noxious stimuli, the cord finds itself unable to handle the increased sensory input and quickly recruits pain-signaling nociceptors. The tiny non-myelinated nociceptors can fast-track sensory messages to the thalamus, warning the brain of the possibility of actual tissue damage. Typically, the brain reacts by layering the affected area with protective muscle spasm. This marks the beginning of stubborn pain/spasm/pain cycles that refuse to be broken until the forward-head posture is improved and normal proprioceptive activity restored.
Interestingly, excessive cortical stimulation causes recruitment of specific sets of muscles “hard-wired” to fire in a predetermined order to guard the vulnerable area. Unfortunately, the first muscles enlisted are often the very same tissues responsible for creating the head-forward posture to begin with; namely, the sternocleidomastoids (SCMs), suboccipitals and anterior scalenes. As these highly innervated soft tissues tighten and shorten, the head and neck are drawn even farther forward resulting in increased myospasm and protective guarding. The brain quickly calls up the next battalion of troops to help counter this intolerable forward-head drag. Below is a brief analysis of typical muscle imbalance patterns resulting from this tenacious battle.
Deeper structural impact
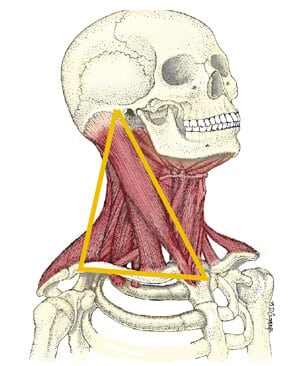
Sagittal plane observations shown in Figure 2 illustrate a guy-wire arrangement of cervical antigravity muscles that, when working properly, allows the neck and head optimal structural support through what is termed a “dual-tent” system. This anterior/posterior cervical muscular support configuration was first described by Joseph Maynard, D.C., in the early 1950s1. His keen observations compared the neck’s anatomy with the balanced guy-wire arrangement of the common four anchor camping tent. Although, the dual-tent system embodies only a small piece of the neck’s elaborate counterbalancing architectural mechanism, this anatomical model best describes the primary support system responsible for protecting the brain’s delicate neurological contents.
One can easily visualize why the brain might recruit the broad splenius capitis muscle to anchor the neck posteriorly due to the shared (front and back) attachments with the SCMs at the mastoid. With this arrangement, the splenius capitis offers a perfect counterforce to the powerful anterior pull of the SCMs.
The levator scapulae are also high on the recruitment list due to their common front/back attachments with the anterior scalenes at C1-C4 transverse processes. This design offers perfect resistance from the constant drag of typically hypertonic anterior scalenes. When working properly, the antigravity function of this four-muscle, dual-tent system is ideal in allowing the human head to gracefully balance on the neck. However, when structural integrity fails due to traumatic changes, the neck’s intricately designed antigravity springing system loses out to compressive gravitational forces acting on it. As cervical curve diminishes, the weight burden falls to deep spinal tissues such as apophyseal joints and intervertebral discs… the devastating beginning of what the medical profession loosely calls degenerative disc disease.
The silent nerve compression syndrome
Biomedical researchers today agree that most neck pain does not directly result from the pinching of nerves. Instead, pain slowly develops from increased stimulation of nociceptors due to compressed and/or inflamed spinal soft tissues, such as ligaments, joint capsules, intervertebral discs, fasciae, and deep transversospinalis muscles.2
Therapeutic client outcomes will dramatically improve once posturally minded pain management therapists begin shifting blame away from pinched nerves and begin incorporating a broader approach that includes pain generated by the sensory receptor system. In a majority of cases, the therapist’s intent should focus on creating myofascial balance, improving posture and restoring joint play to calm hyperexcited sensory receptors in soft tissues forming from the mesoderm.
Although most researchers today dismiss the nerve root as a pain-generating structure due to the lack of positive, objective signs (such as paresthesias, sensory deficits and motor loss), its importance in the pain-management picture cannot be completely overlooked. Loss of disc height combined with vertebral foramina bone spurring can eventually deform and tether the nerve root. As the dural sheath and surrounding capillary beds undergo prolonged mechanical deformation, ischemia, intraneural edema, and loss of axoplasmatic flow of vital nutrients break down axons and pain ensues. Some biomedical researchers3 estimate that 10-15 percent of clients presenting with this type of chronic neck pain suffer from what has been termed the silent nerve compression syndrome.4
Curves, the jaw, and posture
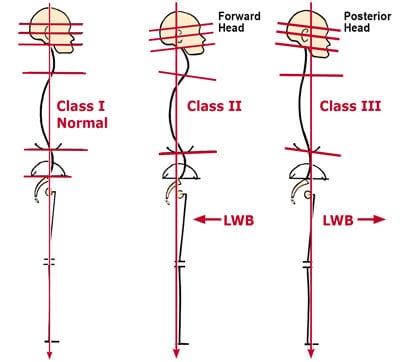
One of the primary postural goals for today’s manual therapist is restoration and maintenance of proper vertebral curves. The contours of the vertebral column exist for a reason: to provide the least amount of strain to muscles, tendons, ligaments and joints so they can carry on with daily chores. If compromised in any way, the risk of future injury and development of pain/spasm/pain CYCLES seriously escalates. To enhance forward-head posture assessment, it is beneficial to include jaw deviation in the equation, since the two are so intimately related. Any alteration in head/neck/thorax symmetry also profoundly affects jaw alignment. The four most common types of neck-and-jaw (Figure 3) relationships are categorized as follows:
Class I, Normal Class II, Retrusive Jaw = Extensor-dominant (ED) neck Class III, Protrusive Jaw = Flexor-dominant (FD) neck Class IV, Retrusive Jaw = Capital extensor-dominant (CED) neck
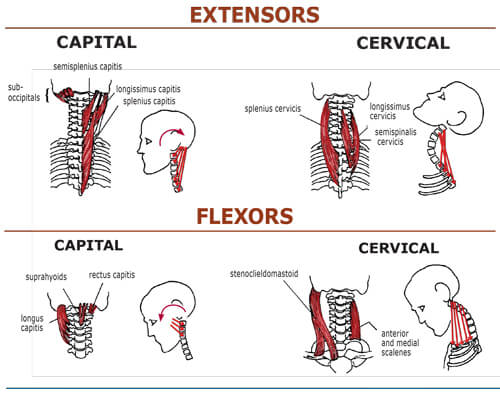
Figure 4 lists various anterior and posterior cervical muscles responsible for creating aberrant Class II and III distorted postures. One can easily visualize how hypertonicity in any of these capital and cervical extensor and flexor groups could initiate asymmetric head, neck and jaw disorders. The following is a brief analysis of three major types of neck/jaw postures. (In the next installment of this 2-part series, a very common and often debilitating forward-head posture, Class IV, will be described and various treatment options presented.)
Although the brain still maintains sustained suboccipital contraction to cock the head back to level the eyes, the extensor-dominate neck’s facet joints actually start hyperextending at C4-5. Upper cervical-complex pain patterns are common, as the superior facet cartilages collide with their inferior counterparts during forced backward-bending. (Headaches occur in Class Hs but are a bigger problem in the Class IV neck due to neural and vascular compression as the head hyperextends through the O-A joint.)
Class I, normal
Optimal upper-quadrant symmetry requires that the heavy head be balanced evenly on the subtle neck so the eyes maintain a leveling with the horizon. In this relaxed position, the jaw and cranial base are perfectly aligned in the transverse plane.
Class II, retrusive jaw, extensor-dominate neck

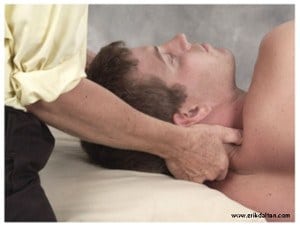
Regrettably, extensor-dominate neck-bowing also moves the head forward in the sagittal plane, usually leaving the jaw behind due to the strong posteroinferior pull of tonic hyoid and digastric muscles (Figure 5). Recall that the cranium and the jaw form from separate myotomes at birth. The jaw belongs to the visceral system, not with the cranium. Although capital and cervical extensors certainly aren’t the only muscles responsible for creating Class II retrusive jaw postures, the brain prefers recruiting these tissues first, due to their resilient ability to battle gravitational forces determined to yank the head down on the chest. Figures 6 and 7 demonstrate two very effective techniques for correcting extensor-dominate necks and associated TMJ problems.
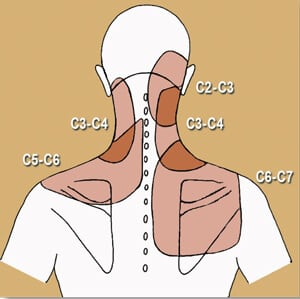
Consequently, the facet’s articular cartilages are required to bear more of the heavy head’s weight. Facets are possibly the most innervated of all spinal structures and are responsible for most non-dermatomal cervical, scapular and brachial pain syndromes seen in bodywork practices today. Figure 9 introduces a facet-pain referral map which helps clinicians immediately identify specific areas where cervical dysfunction may originate.5 Clinical success rates dramatically improve as therapists learn to identify and release short head/neck extensor muscles, while creating tone in overstretched cervical flexors.

When compressive forces dehydrate and flatten cervical discs, the posterior longitudinal ligament becomes lax. Micro- and macro-traumas begin tearing away ligamentous fibers from their firm attachments at the vertebral bodies and disc margins, allowing internal pressure (within the bone) to fill the tiny cracks with calcium. This is the precursor to foraminal nerve-root occlusion and spinal stenosis. Local ligamentous laxity is the primary reason C4-5 and C5-6 discs suffer the greatest number of herniations and are the most operated on of all cervical segments. Osteophytic bone spurring also likes to deform the non-synovial Joints of Von Luschka. When these tiny structures (designed to safely guide nerve roots away from the neck) fill with calcium and hypertrophy, clients often suffer paresthesias, sensory deficits, motor loss and radicular pain syndromes.
The facet and disc dilemma
A devastating chain of pathologic events occurs as hypertonic extensor-dominate muscles fight to level the eyes against the horizon. In clients presenting with excessive cervical curve, the posterior intervertebral disc fibers flatten (at the apex), forcing the superior facet joint to approximate its inferior neighbor. Facets and discs are coupled and interdependent. Facets are possibly the most innervated of all spinal structures and are responsible for most non-dermatomal pain syndromes seen in clinic today. Cervical or lumbar hyperlordosis flattens posterior inter-vertebral disc fibers forcing the superior facet joints to approximate and compress their inferior neighbors. Local hypermobility problems arise at the apex of the curve resulting in ligament laxity, bone-spurring, and disc degeneration.
In Class II ED necks, the therapist will palpate hypertonicity, fibrosis, and myospasm in some or all of the following structures:
- Suboccipitals (rectus capitis major and minor)
- Semispinalis wapitis / cervicis
- Splenius capitis/cervicis
- Longissimus capitis/cervicis
- Ligamentum nuchae
- Suprspinous ligaments
- Upper trapezius
- Levator scapulae
- Sternocleidomastoid
- Hyoids
- Digastrics
- Massater
- Temporalis
References
- Maynard, J. Healing Hands, Foreman Dowling Press, pgs. 219-221, 1991
- Korr, I.M. “Clinical Significance of the Facilitated State,” JAOA 54:277, 1955
- Garfin, S.R., et al. “Spinal Nerve Root Compression,” Spine 20:1810, 1995
- Wilberger, J.E.; Pang, D. “Syndrome of the Incidental Herniated Intervertebral Disc,” Journal of Neurosugery 59:137, 1983
- Bogduk, N.; Marsland, A. “The Cervical Zygapophysial Joints as a Source of Neck Pain,” Spine 13:610, 1988
On sale this week only!
Save 25% off the Upper Body Course!
NEW! Enhanced video USB format!!!
Learn unique approaches to work with the shoulder girdle, arms, neck, and torso, this course will prepare you to relieve painful myoskeletal issues in the upper body. Through video demos and animation, you’ll learn to identify several compensatory movement patterns and their associated reflexogenic pain. With this understanding of where the true source of problems arise, you’ll be able to develop highly effective treatment protocols and deliver lasting results. This course provides you with the skills you need to confidently relieve pain issues in the upper body. (20 CE)
Bonus: When you order the Home Study version, get the eLearning course and and an additional 2CE Ethics eCourse for free!
Save 25% off the Upper Body Course this week only. Offer expires Sunday, March 1st. Click the button below for more information and to purchase the course for CE hours and a certificate of completion to display in your office.