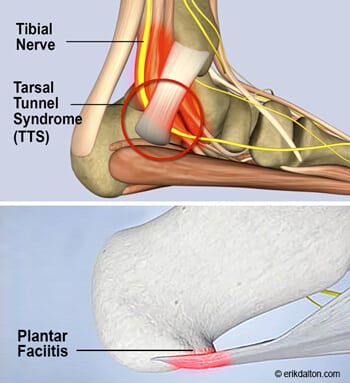
Tarsal tunnel syndrome (TTS) or posterior tibial neuralgia is often mis-assessed as plantar fasciitis as pain in either case arises from medial part of the heel (Figs 1). The symptoms common to both are numbness and tingling sensations, yet the primary symptom that sets them apart is the sometimes-excruciating tibial nerve pain felt at night. True plantar fasciitis sufferers typically report stabbing pains during the first few steps upon arising from a seated position.
The plantar fascia and underlying muscles and sensory neurons are part of an eloquent tensegrity spring system that uses a windlass mechanism to effectively absorb shock and spring us upward and onward (Fig. 2). Yet, loss of anti-gravity spring may cause tissues of the arch to become irritated and inflamed. Biomechanical faults such as hyperpronation or training flaws such as a sudden increase in training mileage may injure the plantar fascia. Prolonged pronation during walking or running causes immense pressure not only on the plantar fascia but also on the posterior tibial nerve as it makes it’s way through the tarsal tunnel.
A known consequence of nerve injury is increased mechanosensitivity. This occurs when mechanical stress applied to a damaged nerve evokes impulses and pain more easily than usual. Nerves that are exposed to excessive or repeated mechanical force become hypersensitive and produce impulses in both afferent and efferent directions. Afferent impulses may promote pain and efferent neurons often cause inflammation in tissues innervated by the sensitized nerve. This injury process is called neurogenic inflammation.
TTS may be assessed and treated in a number of ways but the straight leg raise with dorsiflexed and pronated foot (and a little ankle eversion), seems to work best for me. MAT assessment typically begins with palpation for tenderness at the calcaneal tuberosity and then the straight leg raise test. Rather than tractioning to stretch the nerve, the logical treatment for improving venous flow and oxygenation is to gently glide the nerve. The controlled amplitude of movement during the straight leg raise maneuver should be sufficient to ‘milk’ the nerve, freeing it of congestion. The tibial nerve mobilization video below shows a simple and practical nerve gliding approach for dealing with TTS.
On sale this week only!
Save 25% off the Upper Body Course!
NEW! Enhanced video USB format!!!
Learn unique approaches to work with the shoulder girdle, arms, neck, and torso, this course will prepare you to relieve painful myoskeletal issues in the upper body. Through video demos and animation, you’ll learn to identify several compensatory movement patterns and their associated reflexogenic pain. With this understanding of where the true source of problems arise, you’ll be able to develop highly effective treatment protocols and deliver lasting results. This course provides you with the skills you need to confidently relieve pain issues in the upper body. (20 CE)
Bonus: When you order the Home Study version, get the eLearning course and and an additional 2CE Ethics eCourse for free!
Save 25% off the Upper Body Course this week only. Offer expires Sunday, March 1st. Click the button below for more information and to purchase the course for CE hours and a certificate of completion to display in your office.