Many manual therapists see a rise in injuries and pain as the summer months approach. Those weekend tennis, golf and softball players are getting back into activity after a winter of couch surfing.
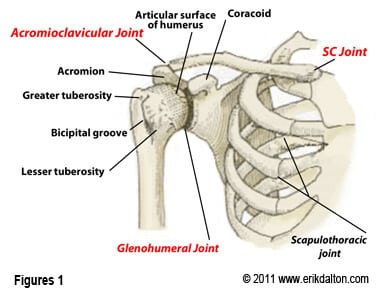
Many who have attended my Myoskeletal Therapy CE workshops have learned a protocol I use in my private pain management practice. Most sessions begin by assessing and treating length-tension imbalances between tonic and phasic (tight-weak) muscle groups. By correcting musculo-fascial imbalances between fast and slow-twitch tissues, distorted posture and movement patterns that alter the position and function of spinal and extremity joints can be more easily addressed (Fig 1). Once trunk stability is established, upper extremities can be evaluated. I’ve found that correcting joint restrictions prior to deep tissue or myofascial mobilization work often offers better clinical outcomes. Fortunately, a quick and easy joint mobilization routine has emerged that compliments both deep tissue and functional movement therapy. This articular stretching technique (AST) enhances daily movement patterns and enhances athletic and sports performance by reprogramming aberrant myo-movement programs responsible for pain/spasm/pain cycles.
When altered joint function disrupts muscular function (and vice-versa), a self-sustaining chain reaction ensues. Passively stretching tight, inert capsular tissues such as frozen shoulders or adhesive hip capsules usually only addresses one piece of the stiff capsular problem. Proper functional strengthening and joint mobilization are also integral pieces of the oft-overlooked pain puzzle.
Active stretching applied frequently to ‘cross-linked’ fibrous tissues found in frozen shoulders, helps reinforce available ROM gained during joint mobilization maneuvers and, if pain is present, should be initiated prior to functional strengthening. I’ve had good success using active “mobilization with movement” maneuvers to damaged, motion-fixated hips and shoulder capsules. Active movement psychologically reinforces to the client that she can move the arm through a greater range of motion (Figs 2, 3, 4). Physiologically, active movement not only assists in healing collagen tissue allowing it to align itself along normal stress lines, but also aids in restoration of normal strength. Active movement also nourishes articular cartilage and enhances repair of damaged tissues.
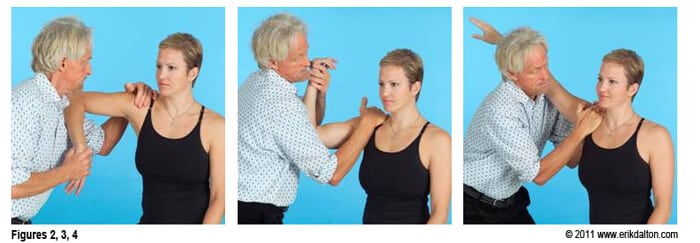
Figure 1: Assessing for Internal Rotation Restrictions
To test for limitations in internal rotation the therapist’s left hand braces medial to the A/C joint, shoulder braces elbow, and his right hand brings client’s arm to the first internal rotation barrier. The client attempts external rotation (pushes up) with a 20% effort to a count of six and relaxes. The therapist then brings the arm down into more internal rotation to the next restrictive barrier and repeats the same procedure until full 90 degrees of internal rotation is restored.
Figure 2: Assessing for External Rotation Restrictions
The therapist’s right hand braces the AC, arm braces the elbow, and his left hand brings client’s arm to the first external rotation barrier. Therapist resists clients attempt to internally rotate (pushing arm down) to a count of six and relaxes. Client’s arm is then brought up to meet the new external rotation barrier and procedure is repeated until 90 degrees of external rotation is achieved. The key to success in this maneuver requires that therapist always maintain the arm in 30 degrees of horizontal adduction so the glenohumeral does not come into play.
Figure 3: Testing Arm Abduction
Now it is time to test the ability of the arm to abduct in a smooth 180 degree pain-free arc. In this test, the client’s right arm rests on therapist’s left shoulder and is brought into 30 degrees if horizontal abduction. Therapist bends knees and hands grasp medial to the acromion. As the therapist slowly straightens his legs while bracing with his hands, a counter-force is created that brings the client’s arm to the first abduction restrictive barrier. Client is asked to press down on therapist’s shoulder to a count of six and relax. Therapist again straightens legs bringing client’s arm up to the new restrictive barrier. This continues until 180 degrees of smooth, pain-free abduction is attained.
It is crucial that normal mechanics of each joint articulation of the shoulder, arm and hand be clearly understood in order to restore full range of motion to injured joints and associated soft tissues (see attached video). In joint mobilization, the focus falls on arthrokinematics—motion occurring at the joint surface, instead of osteokinematics, or bone motion. Each joint within the shoulder girdle has unique arthrokinematics that contribute valuable components toward full shoulder mobility. Each specific joint motion should be considered in the evaluation of any client/patient presenting with restricted range of motion.
The Myo-Skeletal Kinetic Chain
For example, during a tennis serve, the power generated by the shoulder must follow a specific kinetic chain beginning with power produced by the legs, trunk and back. Since the muscle mass of the shoulder is relatively small, if inadequate momentum is generated by the preceding links in the kinetic chain, the shoulder has to play ‘catch-up’ and generate power rather than acting as a force regulator. Improving muscle/joint function in the legs, lumbars and trunk stabilizers, allows reduction of the incidence of rotator-cuff, ligament, and joint capsule injuries.
In my practice, I have come to realize that many shoulder, arm and hand complaints are caused by a lifetime of micro-stresses and injuries to joints. As the brain develops ‘maps’ of the injured ligaments and joints, protective reflex muscle guarding may be sent to splint the vulnerable area. To down-regulate hyperexcitibility in articular mechanoreceptors, it is helpful to begin each upper extremity session with a quick and practical 10-minute joint mobilization routine followed by a thorough evaluation of associated soft tissues. As seen in my Myoskeletal Techniques, Volume III videos, treatment begins with a systematic assessment of all bony articulations in the shoulder, elbow, wrist, and hand starting with the sternoclavicular (SC) joint. This protocol allows me to identify motion-restrictions in soft tissues and joint structures simultaneously. While evaluating each joint, I look for ART:
* Asymmetry;
* Restriction of Motion; and
* Tissue Texture Abnormalities.
Therapist-assisted mobilization routines not only help identify and correct bony restrictions (and create joint-play), but also address extremity pain commonly blamed on soft tissue injuries. Of course, pelvic and trunk alignment and stabilization routines presented in Myoskeletal Techniques Volumes I, II and IV are always performed prior to upper extremity work. The necessity of a combined structural, myo-mechanical and functional approach is a fresh and welcome protocol for all pain, sports, and structural integration therapists.
The reflexogenic relationship of muscles and joints is at the core of the myoskeletal method. Biomechanical analysis of specific joints is not difficult and can help rule out suspected soft tissue injuries. In skilled hands, joint mobilization via articular stretching is a crucial and effective element in injury rehabilitation and prevention.
On sale this week only!
Save 25% off the Upper Body Course!
NEW! Enhanced video USB format!!!
Learn unique approaches to work with the shoulder girdle, arms, neck, and torso, this course will prepare you to relieve painful myoskeletal issues in the upper body. Through video demos and animation, you’ll learn to identify several compensatory movement patterns and their associated reflexogenic pain. With this understanding of where the true source of problems arise, you’ll be able to develop highly effective treatment protocols and deliver lasting results. This course provides you with the skills you need to confidently relieve pain issues in the upper body. (20 CE)
Bonus: When you order the Home Study version, get the eLearning course and and an additional 2CE Ethics eCourse for free!
Save 25% off the Upper Body Course this week only. Offer expires Sunday, March 1st. Click the button below for more information and to purchase the course for CE hours and a certificate of completion to display in your office.








