What’s a neck crick?
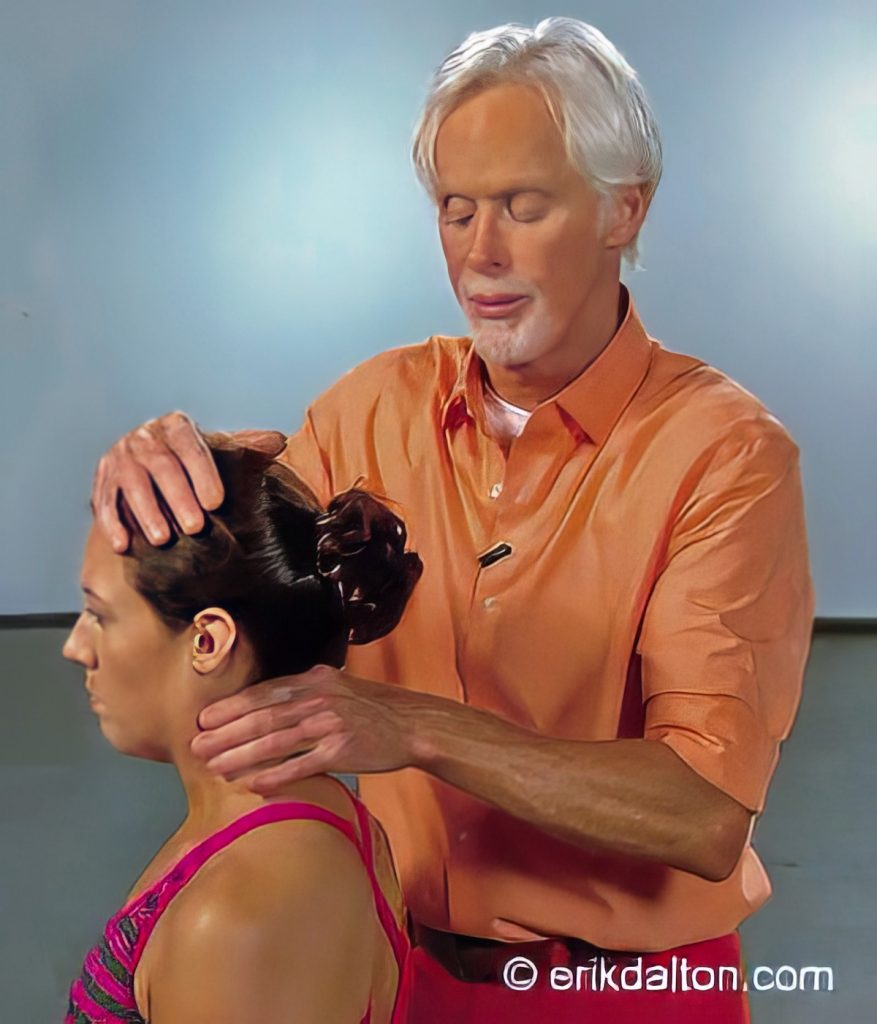
A “crick in the neck” is one of the most common complaints manual therapists hear. The term can describe anything from mild stiffness and loss of motion to sudden, sharp pain that limits even the smallest head turn. When assessing clients with neck cricks, therapists trained in Myoskeletal Alignment Techniques (MAT) engage both the body and the nervous system, using active and passive movements to evaluate range of motion, tissue tone, and pain referral patterns.
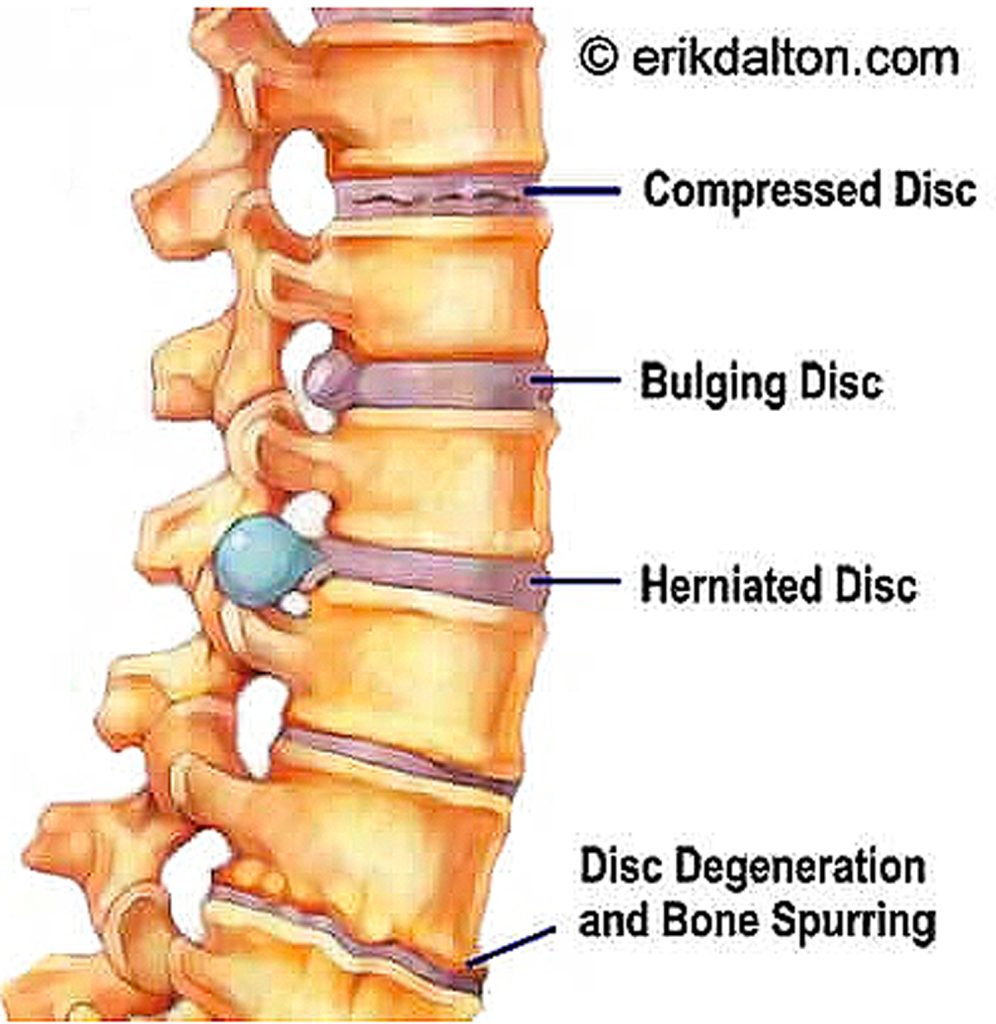
During intake, it’s not unusual to hear that clients have been diagnosed with osteoarthritis or degenerative disc disease and believe those findings explain their pain. While those terms sound ominous, they are usually part of the natural aging process of the spine. Depending on how the brain interprets these changes, they may or may not be actual pain generators.
Clients often link imaging results directly to symptoms, which can heighten anxiety and fear. When working with these individuals, it’s essential not to dramatize or catastrophize. Avoid words or imagery that might trigger worry or reinforce the idea that the spine is “worn out.” The therapist’s calm, confident communication can help prevent the nocebo effect, where negative expectations amplify pain and tension.
This doesn’t mean therapists should shy away from anatomy or orthopedic knowledge. The more you understand spinal mechanics and pathology, the better equipped you are to interpret what you feel and see. Let’s look at how a simple neck crick can evolve from mechanical restriction to chronic pain, and where manual therapy can help change that course.
Stage 1: Mechanical Restriction
A crick often begins quietly. The client notices mild stiffness or a loss of motion, but no real pain. At this stage, joint capsules, ligaments, and deep stabilizing muscles have lost some of their ability to glide and coordinate. Specialized sensory receptors called mechanoreceptors detect this irregularity and alert the spinal cord that something isn’t moving as it should.
The spinal cord responds by recruiting righting reflexes, neurological adjustments that pull the head and spine back into vertical alignment. These reflexes may restore temporary balance, but the underlying restriction remains. Over time, the small intersegmental muscles that control fine cervical motion, like the rotatores, intertransversarii, and multifidi, can fatigue, leaving the neck more vulnerable to sudden locking or cramping.
Stage 2: Inflammatory Escalation
As stiffness persists, joint compression and muscle tension increase. Prolonged stress on the vertebral joints can lead to disc compression and cartilage wear, irritating surrounding tissues. The body responds with inflammation, a natural healing mechanism that, when prolonged, becomes a source of irritation itself.

Chemical irritation triggers chemoreceptors, which join the mechanoreceptors in sending a steady stream of distress signals to the spinal cord. This barrage of information creates a feedback loop of tension, guarding, and more stiffness.
During this phase, clients may describe waking up with a stiff or locked neck, or finding that simple movements like reversing a car or checking blind spots cause sharp discomfort.
Stage 3: Protective Pain Response
Eventually, the cumulative mechanical and chemical signals overwhelm the spinal reflexes. The nervous system calls in its highest level of protection: nociceptors, the body’s danger receptors. These send fast-track messages to the brain, signaling a possible threat to tissue integrity.
The brain then evaluates the situation based on past experience, emotional state, and perceived danger. It may choose to ignore the input, tighten muscles to immobilize the area, or generate pain to encourage rest and protection.
At this point, pain becomes less about the tissue itself and more about how the brain interprets the information. The therapist’s role is to help calm this protective loop by reintroducing safe, controlled movement and restoring sensory confidence.

Re-educating the Nervous System
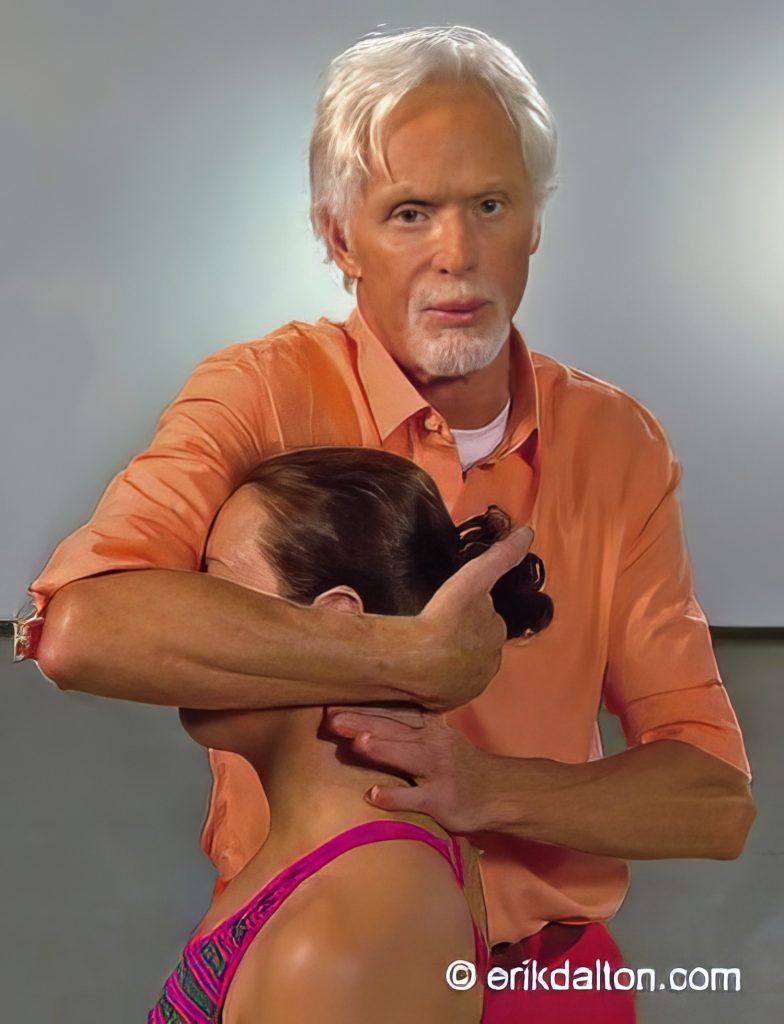
Once pain takes hold, many clients develop sensory motor amnesia—the brain’s tendency to forget how to fully relax or coordinate certain muscles. MAT techniques use graded exposure, gentle traction, and active client participation to retrain these forgotten pathways.
The process is simple but powerful: the therapist moves just to the edge of restriction, encourages small, pain-free contractions, and invites the nervous system to rediscover its range. Over repeated sessions, the brain begins to associate movement with safety instead of threat.
This approach can gradually restore smooth motion, reduce guarding, and improve posture without triggering flare-ups. Clients often notice not only less pain but a sense of freedom and fluidity that extends through the shoulders and upper back.
Helping Clients Understand Their Crick
When discussing a neck crick with clients:
- Normalize it. Explain that mild joint or muscle stiffness is common and not necessarily harmful.
- Reassure, don’t alarm. Avoid attributing pain solely to “degeneration.”
- Encourage movement. Gentle stretching, rotation, and awareness of head posture between sessions can prevent recurrence.
- Focus on safety. Every small, comfortable movement reinforces the brain’s trust in motion.
A neck crick can seem sudden, but it usually follows a predictable pattern: first mechanical restriction, then inflammatory escalation, and finally a protective pain response. By understanding this progression, therapists can intervene early—reducing stiffness before it becomes pain and helping the nervous system reclaim efficient, confident movement.
When we approach neck pain as a conversation between body and brain rather than a structural defect, clients begin to move differently, think differently, and ultimately heal more completely.
On sale this week only!
Save 25% off the Upper Body Course!
NEW! Enhanced video USB format!!!
Learn unique approaches to work with the shoulder girdle, arms, neck, and torso, this course will prepare you to relieve painful myoskeletal issues in the upper body. Through video demos and animation, you’ll learn to identify several compensatory movement patterns and their associated reflexogenic pain. With this understanding of where the true source of problems arise, you’ll be able to develop highly effective treatment protocols and deliver lasting results. This course provides you with the skills you need to confidently relieve pain issues in the upper body. (20 CE)
Bonus: When you order the Home Study version, get the eLearning course and and an additional 2CE Ethics eCourse for free!
Save 25% off the Upper Body Course this week only. Offer expires Sunday, March 1st. Click the button below for more information and to purchase the course for CE hours and a certificate of completion to display in your office.








