The famed Czech researcher Dr. Karel Lewit states: “Respiration is our primary and most important movement pattern… and also the most dysfunctional.” Most clinicians are aware of how breathing affects posture, alignment, and bodily functions, but there is much confusion when it comes to treating underlying joint and myofascial disorders. This blog presents an overview of breathing anatomy, assessment, and treatment strategies to help clients breathe in a more functional and authentic way.
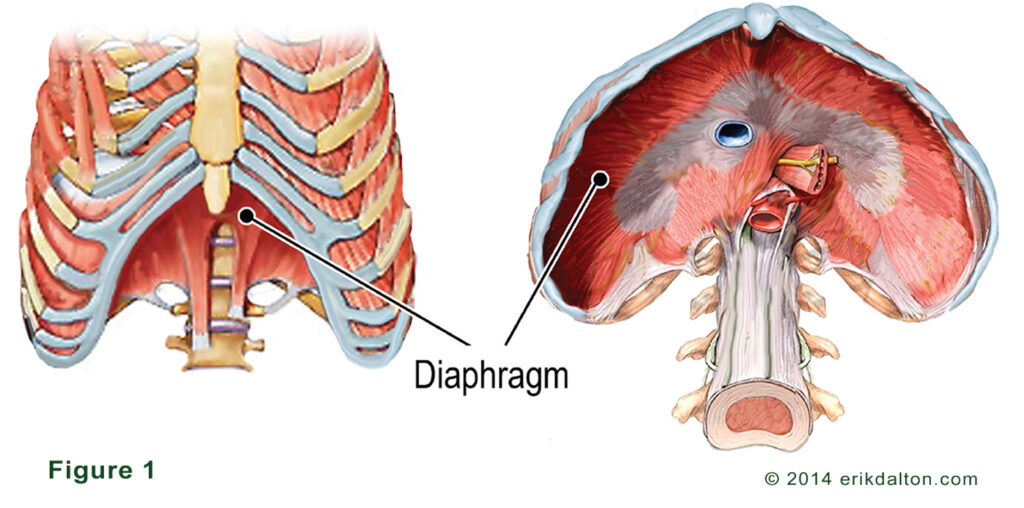
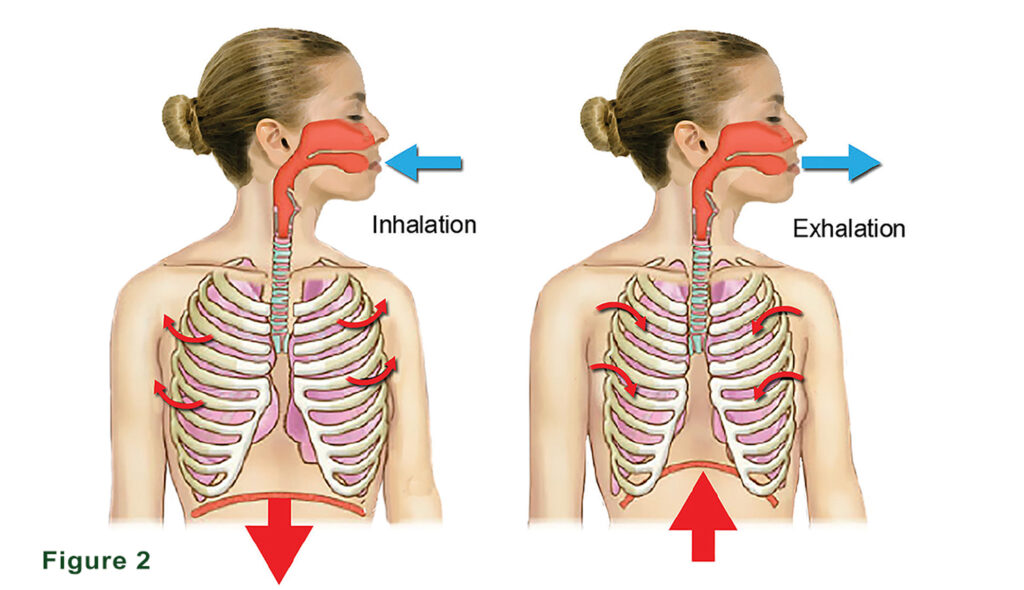
During inhalation efforts, the ribcage has the unique ability to increase its anterior/posterior and lateral dimensions at the same time. The structure most responsible for the generation of negative intra-thoracic pressure is the diaphragm (Fig, 1). Inhalation causes the diaphragm to contract and move inferiorly. This action flattens the dome-shaped muscle causing a decrease of pressure in the thorax and an increase in air taken into the lungs. As we exhale, the diaphragm relaxes, the dome shape is restored, and air space in the lungs decreases causing us to push air out (Fig. 2). Any increase in abdominal pressure via inhalation flattens spinal curves causing an increase in t-spine and ribcage stiffness and stability. Test on your own body.
This involuntary respiratory action works in close coordination with other structures we loosely call the “core”. Because of the intimate relationship between breathing and bony structures, anything that weakens the diaphragm also adversely affects t-spine and ribcage function. And when the body’s joints stiffen, normal breathing patterns suffer. It matters little if you are engaged in a competitive sporting activity, or simply lifting an infant from a car seat, the core muscles must be properly engaged. Dysfunction in any respiratory-related structure makes us more susceptible to pain and injury.
Restoring function reduces the metabolic cost of movement
When tension, trauma and poor posture alter biomechanics and undermine smooth integrated core movement, it is usually easily detectable during gait and palpation examination. Because clumsy uncoordinated movement is less efficient, it alters the body’s loading and muscle activation patterns. Oddly, many chronic pain clients develop ‘movement amnesia’ and are unable to describe or feel alterations in their movement patterns. But, you’ll find the following conditions often go hand-in-hand with a weakened core and loss of proper diaphragmatic breathing:
- Chronic low back pain
- Frequent tension-type headaches
- Emotional system overload, high stress and persistent anxiety
- Chronic postural strain from desk-occupied postures, etc.
- Repetitive and painful rib fixations

A weakened diaphragm causes increased resting tone in upper rib cage muscles such as the scalenes, upper trapezius, levator scapula, and pectorals. The latissimus dorsi and pectorals are not typically thought of as accessory muscles of breathing, but may be recruited in those with paradoxical breathing patterns. This faulty breathing pattern occurs when the abdomen moves in on inspiration and out on expiration and may result in shoulder girdle protraction, forward head carriage, and decreased lumbar lordosis. The accompanying head forward posture causes suboccipital spasm and cervicothoracic pain, as these areas are now asked to bear excessive loads to compensate for the hyperkyphotic t-spine
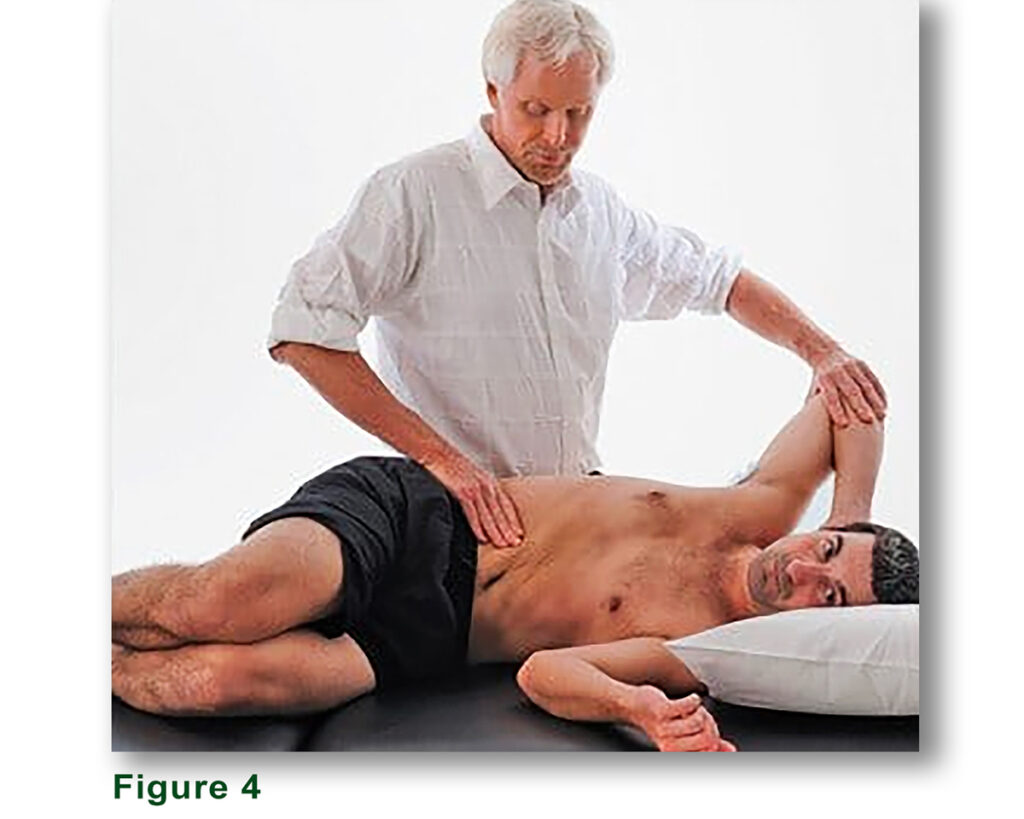
An often-overlooked way of relieving nagging neck, shoulder, or low-back pain is to improve ribcage mobility. In Fig. 3, I demonstrate a (bucket-handle) rib lifting technique. This powerful soft-tissue stretch helps create space between the rib cage and pelvic girdle. In Fig. 4, I activate an inhibited diaphragm while mobilizing the ribcage. As the client inhales, he gently presses his elbow against my hand as I resist to a count of 5. Upon deep exhalation, my fingers work up under the costal cage and pump all the stale air from the diaphragm muscle (repeat 5 times).
The ribcage and core work as a unit and coordinated movement is essential. Depending upon how the brain perceives the threat, pain may manifest when a rib loses its ability to properly coordinate movement with the rest of the ribs and spine as part of a functional unit. This would be similar to a rowing team where one oarsman uses his ore out of sequence with the group. Altered rib function can cause difficulty breathing, restricted shoulder movement, referred pain to other areas, and reactive muscle guarding. Additionally, misaligned ribs can pinch intercostal nerves, sending excruciating pain through the length of the rib and, occasionally, the chest wall (the ole heart attack scare).
It’s virtually impossible to overstate the influence of breathing on t-spine and rib mobility and postural stability. The diaphragm, abdominals, and accessory respiratory muscles produce upward of 21,000 breaths a day. With a strong, freely moving diaphragm serving as the primary muscle for respiration, auxiliary muscles are able to remain soft and relaxed. However, many clients with upper t-spine restrictions (such as a dowager’s hump) breathe primarily with the scalenes and upper scapular fixators (See the treatment and training video above).
Breathing Homework
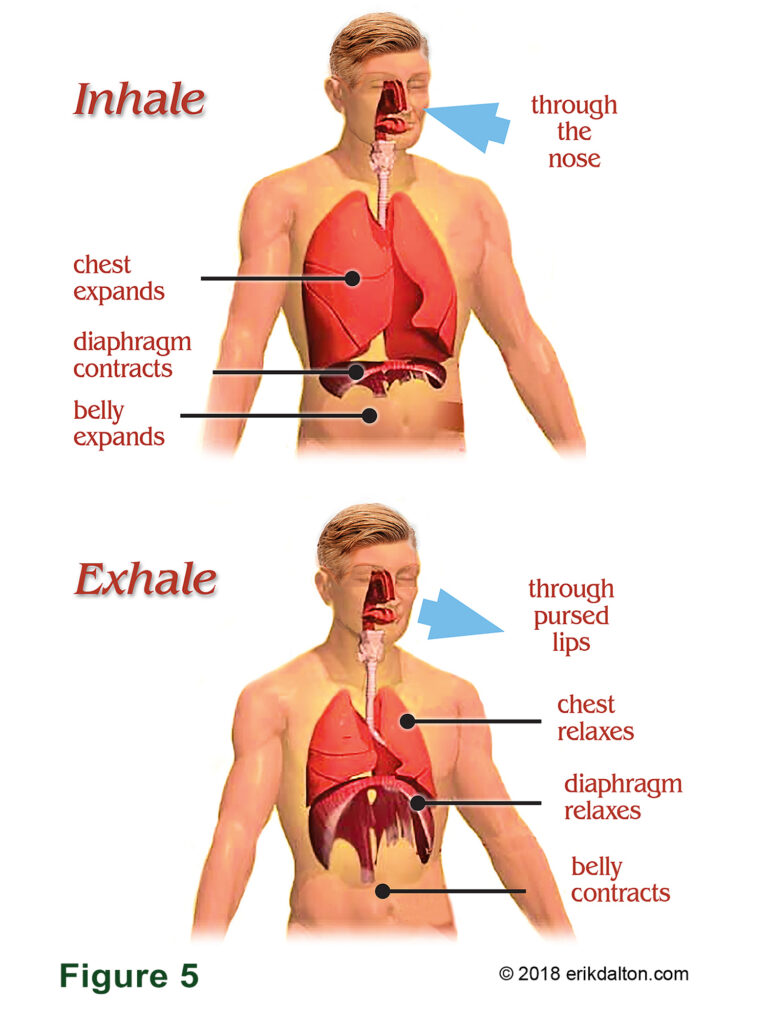
Every client with breathing problems must be given exercise advice. A basic routine I’ve found effective is to have the client place one hand over the lower abdomen and the other on the upper chest wall just below the throat. Instruct them to push the abdomen out as they take a slow, relaxed, full breath in through their nose, and forcefully pull the belly in as the exhale through their mouth (Fig. 5).
As we age and the thoracic spine stiffens, breathing compensations begin. We tend to take breathing for granted because it is so seemingly basic and automatic. Manual and movement therapists are often guilty of neglecting breathing assessment and treatment in favor of more exotic correctional strategies.
But, breathing is one of the most essential innate movement patterns in the treatment of not only spinal stability and myoskeletal pain, but chronic fatigue and anxiety as well. There are numerous techniques and modalities that teach breathing including yoga, fascial fitness and various forms of functional rehab. Treating the dysfunctions and teaching your clients proper ways to breathe are essential for optimal health and athletic performance.







