Clinical reasoning for an evidence-informed practice
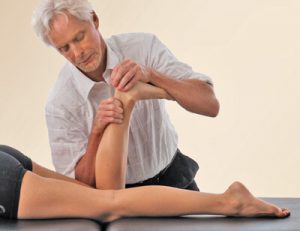
Each of us has a toolbox packed with assessments and techniques for treating clients with various pain complaints. Using clinical reasoning, we can evaluate these practices and apply them effectively. Put simply, clinical reasoning is the process by which a therapist interacts with a client, collects information, and tests a hypothesis to determine an optimal treatment plan. It is a reflective process of inquiry between therapist and client with the aim of understanding more about the context and clinical presentation of the pain. Such understanding, in turn, allows us to build an evidence-informed practice.
Novice clinicians often think all they need are better hands-on skills and more techniques. I agree techniques are the foundation from which to build a strong skill set. However, in a clinical reasoning practice, the goal is to constantly reflect on what we’re doing so we better understand what has or hasn’t worked for our clients in the past. If we don’t reflect on what we’re doing, it will be more difficult to improve future treatment outcomes.
Observation, communication, assessment, pattern recognition, inference, and problem solving are important clinical reasoning skills you’ll need to hone as you work toward an evidence-based approach.
Confronting confirmation bias
The first step toward improved clinical reasoning is to realize we all have blind spots and biases. Most of us do not like to challenge our firmly held beliefs. Not only does it make us uncomfortable, which no one likes, but it also forces us to reconsider what we think we know. The tendency to interpret evidence based on one’s existing beliefs is termed “confirmation bias.”
The way a therapist clinically reasons their findings through assessment and history-taking can strongly influence how a client’s case is interpreted. As we evaluate movement restrictions, gait abnormalities, biomechanical faults, and mental states, it’s important to observe for “red flags” that may give weight to how the pain or injury complaint could have developed. Skilled manual therapists can then apply more accurate anatomical, pathological, and biomechanical assessments to the client’s particular presentation and construct a therapeutically effective treatment plan.
Inductive and deductive reasoning
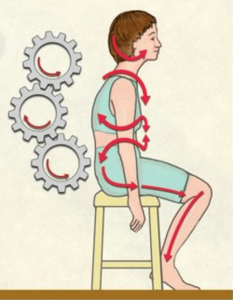
To develop a successful pain-management treatment plan, we begin by using inductive and deductive reasoning. Inductive reasoning is a bottom-up approach that looks at the client’s situation from their point of view through communication. It begins with an observation, supports it with pattern recognition, then arrives at a theory about the client’s problem. For example, “My client Mary has pain down her leg during prolonged sitting. The last two clients who presented with pain down their leg during prolonged sitting were medically diagnosed with piriformis syndrome. Therefore, Mary must have piriformis syndrome.” In this example of inductive reasoning, the theory may or may not be true. To avoid going down the wrong path, we must include deductive reasoning.
Deductive reasoning is a top-down approach that begins with a theory, supports it with observation, and arrives at a confirmation. For example, “The piriformis muscle can compress the sciatic nerve. All Mary’s orthopedic assessments and radiology reports are positive for piriformis syndrome. Therefore, Mary has piriformis syndrome.” In this example of deductive reasoning, the confirmation should be accepted only if the treatment changes Mary’s symptoms.
Just as there are weaknesses with inductive reasoning, there can be flaws in deductive reasoning. The most obvious danger comes in formulating and accepting the major premises. The assumptions must either be so self-evident that no reasonable clinician could possibly object or be ones that can be proven by clinical studies or physical observations as in Mary’s case.
In science, there is a constant interplay between inductive reasoning (based on observations) and deductive reasoning (based on theory) as we get closer and closer to the “truth,” which we can only approach, not ascertain with complete certainty. To get as near as possible to the truth, it is best to use a combination of both deductive and inductive logic. Starting with deductive reasoning, we can formulate a basic premise upon which all else can follow. Then, through clinical studies and inductive reasoning, we can verify the accuracy of that premise.

Information collection is critical
The strategic collection of information plays a key role in clinical reasoning for an evidence-based approach. In the pain management setting, we can collect information about the client’s complaint by asking the following questions:
- How do you think it began (pratfall, sports injury, lifting, failed surgery)?
- Why do you think it hurts (overuse, underuse, abuse)?
- What kind of movements trigger the pain?
- When did it happen? Does the pain come and go? Is it an acute episode or chronic?
- Where do you feel the pain? Can you point to the area with one finger?
Such open-ended questions help us understand the client’s point of view and make observations for inductive reasoning. Remember to keep the inquiry general: “Tell me more about your leg pain,” rather than, “I see your MRI shows a disc herniation. Does your leg hurt when you bend forward?”
After collecting information based on the client’s perception of their pain complaint, we can proceed to yes or no questions that will aid in deductive reasoning. For example: Do you feel pain in your low back? Does your leg only hurt on one side? Does sitting flare your symptoms? Is the leg pain worse when you’re under stress?
When the client’s presentations deviate from commonly seen clinical patterns, try new movements or techniques or exercises. Feel free to improvise if it allows you to explore the presentation further and better tailor the treatment to your client’s specific needs.
Practice makes progress
It is important that massage therapists are taught to understand and apply clinical reasoning in their pain management practices. Fortunately, clinical reasoning skills can be strengthened at any age and experience level. It may be helpful to think of it as studying how the “experts” become experts, then setting yourself on that path of continuous learning. There’s an old saying, “If you have 10 years of experience, you don’t want it to be one year that you’ve lived 10 times.” Instead, you want a decade of experience characterized by a reflective, ongoing inquiry process that drives you to continue learning. Expertise is not a goal we reach — it’s about making continual progress.
On sale this week only!
Save 25% off the "Dalton Technique Treasures" eCourse
The “Dalton Technique Treasures” eLearning course is a compilation of some of Erik’s favorite Myoskeletal Alignment Techniques (MAT). Learn MAT techniques to assess and address specific sports injuries, structural misalignment, nervous system overload, and overuse conditions. ON SALE UNTIL July 29th! Get Lifetime Access: As in all our eLearning courses, you get easy access to the course online and there is no expiry date.