Working with a sensitized nervous system
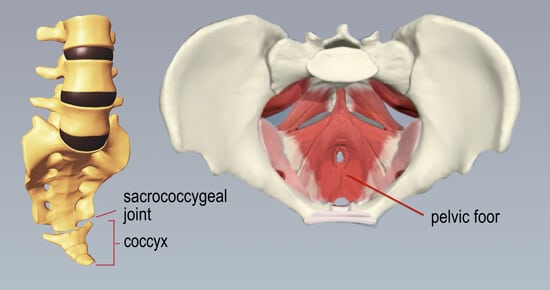
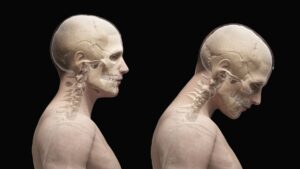
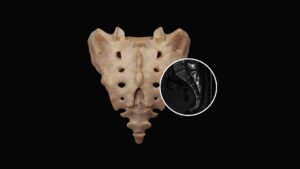
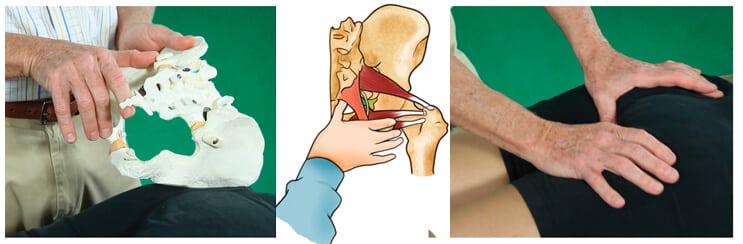
Researchers are uncertain why some people with coccyx dysfunction are symptomatic and others are not, but it’s likely linked to pain gating malfunction and coccyx hypersensitivity. Here, we’ll focus on assessing and correcting the most commonly seen coccyx disorders — sacrococcygeal joint misalignment and accompanying pelvic floor muscle spasm (Image 1.). To begin, let’s review possible causes and symptoms in clients suffering coccydynia pain.
Pratfalls and direct blows to the coccyx from contact sports are obvious culprits, but what about the strenuous compressive forces cyclist, rowers, and desk jockeys place on the tailbone? In this “overuse and abuse” population, spastic pelvic floor muscles over-engage and bind down the coccyx and surrounding neural structures. When noxious input from strained connective tissues overloads the spinal cord’s neuronal pool, the brain gets involved and may decide to splint the area with protective muscle spasm. Thus begins the vicious cycle of muscle overuse causing brain irritation causing more layering of protective spasm.
Overuse injuries and direct blows are not the only contributors to coccyx pain — consider the potential insult the coccyx experiences during pregnancy. At the end of the third trimester, hormonal changes enable the synchondrosis between the sacrum and the coccyx (sacrococcygeal joint) to soften and become more mobile. This increases coccygeal segmental mobility, allowing for more sidebending, flexion, and extension, which is a good thing. However, in some mothers, the resting tension of surrounding musculoligamentous connective tissues is altered as secretion of the hormone relaxin decreases.
Unlike fractures, which can remodel, sacrococcygeal joint injuries can last indefinitely if an inflamed joint is repeatedly forced from its normal position. In cases where inflammatory waste products trigger chemoreceptors and altered sacrococcygeal joint alignment hyper-excites mechanoreceptors, the brain often decides to lock the area up to prevent further insult. This is where myoskeletal therapy may help.
Symptoms and corrections
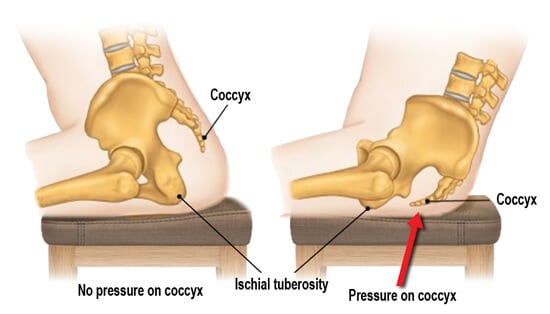
In a fully functioning body, the coccyx acts as a shock absorber by flexing forward during sitting. Together, the coccyx and bilateral ischial tuberosities form a weight-bearing tripod that houses the pelvic floor muscles and ligaments. The coccyx bears more weight when a seated person leans back, so we often see coccydynia clients flex at the hips to shift more weight to the sitz bones (Image 2.). They usually report dull, aching pain emanating from the gluteal cleft just superior of the anus and sometimes stabbing pain when rising from prolonged sitting.
Discussion
Pain is a symptom all healthy human beings experience at some point in their lives. In fact, pain sensation is necessary for survival — without it, we would not know if we were injured or unwell. However, in our sensitized clients, the degree of pain does not always match the degree of injury, and this is where proper manual therapy and corrective exercise can help. Working together in a comfortable, safe environment, we can identify specific movements that reduce a client’s coccydynia symptoms and help eliminate areas of bind. Getting the client moving and exercising is always a great strategy for easing the pain of coccyx dysfunction.
Reference:
1. Lirette, L.S., Chaiban, G., Tolba, R., & Eissa, H. (2014). Coccydynia: an overview of the anatomy, etiology, and treatment of coccyx pain. Ochsner Journal, 14(1), 84-87.
On sale this week only!
Save 25% off the Dalton Technique Tour course!
NEW! USB enhanced video format
Discover deep tissue, pin and stretch, nerve mobilization, and graded exposure stretches in this comprehensive “technique only” program. Upon completion, you will receive 16CE hours and a certificate of completion to display in your office. Save 25% this week only. Offer expires Monday, January 19th. Click the button below for more information and to purchase the course.
BONUS: Order the home study version and get access to the eCourse for free!