Contemporary bodyworkers are blessed with freedoms rarely afforded other professional health care practitioners the three M’s: Minutes, Myofascia and Maintenance.
Let’s Talk Minutes
With most sessions lasting from 45 minutes to 90 minutes, today’s massage and bodywork practitioners are allotted sufficient hands-on time to develop a keen awareness of the client’s ability to function in physical, emotional and spiritual planes. It’s unfortunate for both client and therapist when time constraints (common in many manual medicine practices) become a primary determinant in the success or failure of the therapeutic intervention. Fear of “running late” and anxiety intensified by rushing from one client to another often disrupt a session’s rhythm, preventing the development of physical and mental rapport. Clock-watching is the enemy of attunement, focus and intent as the therapist unconsciously drifts from being totally “present” with the client to suddenly worrying about getting enough “techniques” completed in the allotted time frame.
“Minutes” allows the therapist time to observe, assimilate and record such things as postural abnormalities, present state of mind, painful past experiences (both physical and mental), positive or negative attitudes about their condition, and preconceived ideas about their recovery.
In a relaxed pain management practice, therapists can practice honing such skills as visual screening evaluations, anatomical landmark comparisons, injury assessments and history intakes. This physical examination process can be performed with clients clothed, in bathing SUITS, sportswear, etc. Make it a habit to observe clients as they enter your therapy room. Look for clues by noting how they sit, remove a jacket, lean forward to untie a shoe, or get up from a chair. Clients often reveal more information when performing normal unconscious movement patterns than when asked to actually execute such tasks as walking, forward bending, range-of-motion maneuvers, etc. More truthful patterns often emerge if the clients are unaware that they are being observed.
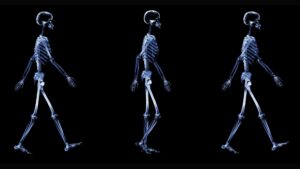
From Essential MAT Assessments course
Since our ultimate therapeutic goal is to establish pain-free movement during the walking cycle, gait evaluations rank high in every assessment protocol. By making mental notes during gait observations and comparing them with anatomical landmark findings, valuable information can be recorded and stored for future reference. Always check for obvious dysfunctions such as short legs, pelvic tilts, low shoulders, cocked heads, scoliotic patterns, etc. With practice, visual and physical assessments can be performed quickly and efficiently, even with the client completely DRESSED. The following is a laundry list of some things to look for during a typical client evaluation:
- holding patterns during gait;
- asymmetrical anatomic landmarks;
- presence of upper and lower crossed syndromes;
- abnormal front-to-back (A/P) and side-to-side (scoliotic) curvatures;
- aberrant muscle-firing order patterns;
- arthritic hands;
- pronated/supinated feet;
- excessive wear patterns on the client’s SHOES; and
- emotional states (extreme anxiety, “bug-eyed,” withdrawn, angry, etc).
When therapists take time to focus, relax and carefully listen to a client’s history during a typical intake session, a clear picture often emerges. Unfortunately, the picture frequently changes from visit to visit as the client recounts past events. So, what is the best way of arriving at a true pain portrait of this individual?
Medical history-taking often is unstable, according to psychiatrist Arthur Barsky, MD.1 “Patients frequently fail to recall (and therefore under-report) the incidence of previous symptoms and events; tend to combine separate, similar occurrences into a single generic memory; and falsely recall medical events and symptoms that did in fact occur,” Barsky explains.
In both acute and chronic neck/back pain clients, history often relates to individual personality characteristics, state of health and mind at the time of recall, and preformed beliefs about symptoms and prognosis. Most manual therapists would agree that clients also are less likely to recount distant events accurately than they are more recent occurrences. Therefore, it behooves today’s manual therapist to consider the following factors when interpreting a client’s history.
Practical intake tips:
1. Establish anchor points or memorable events that might help clients recall their symptoms.
2. Encourage clients to convert generic memories of symptoms into more concrete episodes.
3. Ask clients to recall their symptoms in reverse order, starting from the present.
4. Take the history in a similar way each time.
Questioning clients about events surrounding traumas or work-related injuries during the therapy session often reveals new and helpful insights. The addition of touch not only calms nervous system hyperexcitability, allowing thoughts to flow more freely, but also triggers tissue memory as the injured area is being worked. Accurate, focused assessment is crucial, particularly in chronic cases, since time might have elapsed since the event(s) leading up to the painful condition. Therapeutic outcomes improve dramatically as therapists develop creative, yet consistent methods of helping clients present an accurate portrait of their past and present musculoskeletal health problems.
As mentioned above, the art of history-taking possibly is the most underrated and least appreciated of all therapeutic interventions. A client’s history is never taken but continually updated and expounded upon throughout each therapy session. Effective history-taking develops rapport, while extracting key pieces of pain puzzle information.
During a traditional relaxation massage session, silence is golden. However, in pain management settings, history-gathering via subtle ongoing conversations frequently produces sudden intuitive insights that might prove instrumental in their recovery. Caring therapeutic touch not only forms a bond of trust, but often triggers important suppressed memories. It’s amazing how much key information people tend to forget or are unable to verbalize until you get your hands on them. The more they feel the therapist is emotionally committed to helping solve their ailments, the greater the chances unconsciously blocked information concerning a past injury or stressful incident might resurface.
The therapeutic use of anchors saves time by empowering the therapist with a reference point so clients can be mentally guided back to certain events, injuries, accidents or stressful situations that might have precipitated the pain. We have all experienced the frustration of searching unsuccessfully for that key event that triggers a chronic pain episode when the client suddenly belts out, “I completely forgot about that snow boarding accident my neck began hurting a couple days after that kid knocked me down,” or “You don’t think it had anything to do with the new mattress and pillow, do you?” or “Mom thinks I fake my migraine headaches so I don’t have to go to school, but they didn’t start until I got braces.” Once the therapist establishes reference points, they can be used as anchors during subsequent sessions to secure new insights on the type and cause of the client’s injury or illness.
The key to performing good intakes and evaluations is to listen, listen, listen. Enter each session with open eyes, an open mind, and most of all – an open heart. The goal is in refining and combining intuitive skills with a well-rounded therapeutic background. Touch therapists, especially those specializing in pain management, should begin each session with the open-minded wonderment of a child waiting excitedly to see what the body has to teach you that day. Let the energy systems do the talking and the hands do the walking.
Body-Listening
Body-listening is an art form that, when perfected, clearly guides our therapeutic intent. Entering a session with preconceived therapeutic goals often leads the therapist down a blind path. We often forget it’s the client who knows what is going on in his or her own body, rather than some expert voicing opinions and making decisions on what he or she perceives to be the problem. Because therapist and client interact in many conscious and unconscious ways during a session, body-listening through skillful touch provides the anchor that promotes healthy mutual communication.
Development of clear intent and keen palpation skills provide the keys for unlocking the door to the art of body-listening. Therapists’ hands palpate for many different things. Where one therapist might focus on a client’s aberrant postural patterns, another might be palpating respiratory, cranial or visceral rhythms. Practitioners of myoskeletal bodywork add another dimension by imagining the shifting skeletal architecture as specific deep-tissue structural techniques are applied. Regardless of a practitioner’s personal preference, to truly tune in physically and emotionally, personal communication must be in a form understandable to the cli-ent. The approaches presented in neurolinguistic programming (NLP) best explain how the client and therapist’s inner world of communication might not conform, causing a breakdown of auditory and tactile communication.
For example, the therapist might be stuck in a visual or kinesthetic language exchange with a client who is basically an auditory communicator. It’s helpful for the therapist to listen for clues, both in language and touch, as to the client’s communication preference. For example, if the client frequently uses words like, “I see what you mean” or “It looks like my neck turns better to the right,” the therapist also might try communicating with more visual terms.
The same applies to touch. Oddly, a large number of manual therapists tend to be right-brained, visually dominant communicators, whereas many clients – being hard-core bodywork advocates – lean more toward the kinesthetic side. If the client communicates best from a kinesthetic (tactile) space, the therapist must learn to elevate his or her body-listening skills to better communicate with the special needs of these touch-sensitive clients. Slowing down and working with the client’s ventilatory (breathing) or craniosacral processes helps form an unconscious bond that delights the kinesthetically attuned client.
Myofascia
One reason the massage and bodywork profession continues to grow at a staggering rate is that we have been blessed with specialized training in the most pervasive of all body structures, the myofascial system. This complex neuromyofascial network is the first to exhibit change, and also the first to show dysfunction.
Beginning with superficial structures, the therapist’s fingers, elbows and fists slowly engage the body’s marvelous myofascial web. This neurologic, electrically charged connective tissue matrix is continuous throughout the body. Fascia is not just the gross outer covering of muscles and organs; it’s also prevalent in muscles and organs covering every muscle unit and organ part ultimately impacting the contour of the human body.
Since the myofascial system is composed of dense, regular connective tissues, it falls into a histological category that includes ligaments, tendons, fasciae and aponeuroses. Its MAKEUP consists of collagen fibrils, fibroblasts and elastic fibrils. Fascia both wraps and compartmentalizes the body, the extremities and the muscles via a living web, enveloping the entire physical structure. From this perspective, one can see that fascia possesses the ability to shape the body and its spinal curvatures into either optimal or aberrant postural patterns.
Recall that the myofascial system has virtually no parasympathetic innervation. All soft tissues are innervated by the sympathetic nervous system which, among other things, controls the rate and flow of blood. Since the cardiovascular system has a sympathetic nerve attached to it, the two systems – neuromuscular and cardiovascular – both are regulated by the sympathetic nervous system. When functioning properly, they establish homeostatic balance in the vasomotor system. Obviously, there is a dynamic symbiotic relationship between these two systems.
Because the sympathetic nervous system consumes the greatest amount of the body’s energy, uses more oxygen, and produces the most waste byproducts, it should be regarded as the fundamental underlying system of the body. In healthy individuals, the sympathetic nervous system works in perfect balance with the viscera or enteric nervous system – which is primarily responsible for the digestion of food – to process and produce essential amino and fatty acids as fuel for metabolism.
When the brain’s limbic system or cranial accessory nerves are stressed through tension, trauma and poor posture, an overstimulated myofascial system sympathetically tightens. Soon, protective guarding results in contractures, fibrin deposition and myospasm. Regrettably, increased stimulus to the myofascial system’s neuromuscular component results in decreased visceral activity and resultant sympathetic nervous system dominance.
The myofascial advantage is that it allows therapists to work within this embryologically primitive system, with a goal of bringing balance to muscles and other connective tissues to improve posturally related pain conditions. This leads to a more efficient self-regulating, self-correcting, more adaptive human being. Establishing proper postural balance initiates more refined proprioceptive skills, smoother locomotion during gait, and energy efficiency throughout the entire neuromyofascial system.
Maintenance
When living in an overstimulated society filled with cultural pratfalls such as job-related prolonged sitting, stressful (and often competitive) workplaces, divorces, dysfunctional peer-pressured children, and other family matters, it’s essential that individuals be put on a regular maintenance schedule much like we do with animals, automobiles and medical exams. What better and more evolving thing can people do for themselves and their family than preventive body maintenance?
Long-term observation and experimentation opens the DOOR to innovation. Some of our best training is learned “in the trenches” in a full-time practice. Here we are given the opportunity to see what works and what doesn’t, as each individual brings in therapeutic challenges that mold and hone our skills. Most body therapists discover their abilities improve exponentially when allowed to track and treat clients over a period of time. Being exposed to difficult cases raises the bar and inspires a passion for developing more therapeutic and efficient ways to evolve and rehabilitate those in need.
Over a period of years, a gradual evolution and paradigm shift transpired in my practice that led me to collect a diverse group of like-minded eccentric individuals I really enjoy being around. I am forever indebted to these people for allowing me to nurture, maintain and elevate their physical condition – and mine. These people have become part of my extended family, and I expect to “maintain” them and their families for the rest of our lives.
Each October, as the new appointment book arrives, history intakes are reviewed and progress evaluations conducted. A mutual decision is made as to how much maintenance might be necessary for the following year. Some have pathologies requiring regular, weekly visits; many adhere strictly to home retraining exercises, and are seen monthly or even quarterly. By the middle of December, all of my regular clients have been scheduled, and my appointment book is full for the upcoming year.
In order to accommodate newly referred clients that might just need a quick fix, I keep a waiting list. My regular clients are encouraged to cancel if they are feeling well, monetarily stressed, or have conflicting appointments. This permits new clients to be filtered in, screened and helped if possible. If my schedule does not permit, or their condition seems to fit better with another practitioner, I refer them out. Over time, I have accumulated a broad referral base of complementary medicine providers such as chiropractors, MDs, DOs, PTs, acupuncturists, Rolfers, and other myoskeletal therapists.
For this type of long-term maintenance to be successful, however, an open and honest dialogue must be established early to prevent development of a transference or counter-transference situation. The more knowledge I gather and share from observing my client’s bodies, the more educated they become about their own bodies, which promotes self-reliance. Always erring on the side of modesty has proven the best recipe as far as my own personal comfort level. My work has become much more attuned, relaxed and centered knowing my clients feel safe in the caring atmosphere of my office.
Therapists specializing in pain management require adequate session time to filter the results of the client’s history, palpatory findings, and all other pertinent tests through a physiologic lens formed via the scientific scope of basic science and clinical experience. Recently, there has been a noticeable upsurge of fine therapists entering the pain management field, and for obvious reasons. People feel personally rewarded when helping others in need. But, entering this discipline requires the transition be accompanied by advanced study in palpation skills, assessment, history taking, biomechanics, and pathology. Therapists must resist the temptation to mentally BOX” the client’s complaint into a “fix-it” formula that excludes the body as the primary healer. Fortunately, the human body is not a machine. It possesses the ability to heal with some help from friendly hands and the three M’s: Minutes, Myofascia and Maintenance.
Click here for more information.
On sale this week only!
Save 25% off the Upper Body Course!
NEW! Enhanced video USB format!!!
Learn unique approaches to work with the shoulder girdle, arms, neck, and torso, this course will prepare you to relieve painful myoskeletal issues in the upper body. Through video demos and animation, you’ll learn to identify several compensatory movement patterns and their associated reflexogenic pain. With this understanding of where the true source of problems arise, you’ll be able to develop highly effective treatment protocols and deliver lasting results. This course provides you with the skills you need to confidently relieve pain issues in the upper body. (20 CE)
Bonus: When you order the Home Study version, get the eLearning course and and an additional 2CE Ethics eCourse for free!
Save 25% off the Upper Body Course this week only. Offer expires Sunday, March 1st. Click the button below for more information and to purchase the course for CE hours and a certificate of completion to display in your office.