The Secret Life of Spinal Discs
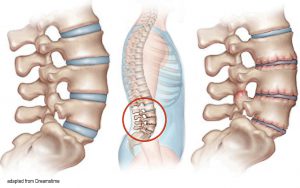
The intervertebral discs are responsible for 25 percent of our spine’s overall length. Given that the average adult spine measures 24 to 28 inches, the intervertebral discs account for six to seven of those inches. In young individuals, the water-filled, gel-like nucleus pulposus and annulus fibrosis are both firm and flexible. However, by age 40 — earlier than any other connective tissue — the vertebral discs often begin showing degenerative changes (Image 1). 1 As the disc dehydrates and loses elasticity, the length of the spinal column can shrink by three centimeters or more. Thus, most of us get shorter as we age. To resist gravity’s compressive forces, the myoskeletal method uses graded exposure stretches to ease protective guarding, neurologically awaken anti-gravity muscles, and help restore lost body height.

In a study titled “Nutrition of the Intervertebral Disc,” a team of researchers from Oxford University found that loss of nutrient supply can lead to cell death, as well as an increase in matrix degradation and disc degeneration.2 Oddly, vertebral discs are among the few human tissues that do not possess an independent blood supply. Even our teeth, nails, and hair extensions have designated nutritional vessels, but the discs do not. The annular fibers require glucose for survival, and the nucleus obtains fluids and eliminates waste — primarily lactic acid — through a complicated process called imbibement. The imbibing of water occurs as individual spinal segments flex, extend, sidebend, and rotate during normal daily activities.
Contrary to popular thinking, vertebral discs are not designed to act as the spine’s primary shock absorber. This role belongs to a marvelously designed musculofascial spring system. Notice in Image 2 how the flexible colored bands, which represent muscles and ligaments, form a tent-like tensegrity arrangement. When healthy, these soft tissues can maintain separation of vertebral bodies even with the disc completely removed. Equipped with these facts, we’re left with this question: If restoring anti-gravity function is the key to slowing spinal disc aging, then what’s the best way to pump those discs up?
Fetal positioning and imbibement

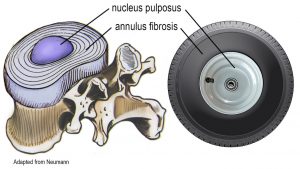
When picturing an intervertebral disc, most of us think of the outer annular fibers as circular connecting rings, similar to a radial tire, that support the gel-filled (hubcap) nucleus. However, many of the disc’s concentric tree-ring fibers do not connect, nor is the disc round (Image 3). Mother nature cleverly thickened the anterior and lateral sides, leaving the thinner posterior fibers to absorb lubricating fluids during daily activities and also during sleep. Strangely, 80 percent of this fluid imbibement occurs during the first hour of sleep. That’s why researchers believe the best resting position for rehydrating discs is a sidelying fetal position with knees flexed, chin tucked, and lumbar lordosis flattened. This trunk and hip flexed fetal position opens the posterior compartment, allowing the thinner disc endplates to suck in water to nourish the disc.

The downside to this type of disc design is the increased risk of disc herniation due to lack of posterior fiber integrity.3 Still, there’s hope for damaged discs. A 2017 study found that conservative care fosters the drawing in of some disc bulges and may help relieve sciatic nerve root compression.3 Gentle pain-free hyperextension exercises, such as the cobra yoga pose, are often used to relieve posterior nerve root compression by moving the nucleus anteriorly. However, I have experienced greater success performing fetal tractioning maneuvers and client-assisted stretches, such as the ones demonstrated in Images 4-6. Delivered throughout a series of sessions, these lumbar-pumping maneuvers appear to increase fluid absorption and aid in body height restoration.

Recently, I’ve begun using an accurate measuring device to track client height during intake and again after several sessions. I find this tracking routine acts as a novel stimulus that helps keep both client and therapist engaged in the process. To enhance the therapeutic outcome, I encourage clients to perform a variety of movements on their own time, from swimming and mini-trampoline bouncing to tai chi and hiking. These playful activities, when combined with myoskeletal therapy, bring awareness to movement “blind spots” and help clients break non-optimal movement patterns.
Summary
In sports and recreation, a healthy anti-gravity musculofascial system transmits and releases stored elastic energy from the ground up through the individual spinal segments, causing them to spring open and hydrate the vertebral discs. To relieve protective muscle guarding, restore anti-gravity function, and bring some lift to the body, I’ve found success using therapeutic stretching and manual spinal tractioning in a controlled, comfortable manner. Corrective exercise also aids in reducing protective muscle guarding and restoring body height as water and nutrients are pumped into injured and spasmodic muscles, ligaments, and intervertebral discs. Not only will your low back benefit, so will your golf swing, along with your ability to walk, run, climb, lift your children, and simply stand tall.
Notes
1. Urban, J., & Roberts, S. (2003). Degeneration of the intervertebral disc. Arthritis Research & Therapy, 5(3), 120-130.
2. Urban J.P., Smith, S., & Fairbank, J.C. (2004). Nutrition of the intervertebral disc. Spine, 29(23), 2700-2709.
3. Altun, I., & Yüksel, K.Z. (2017). Lumbar herniated disc: spontaneous regression. Korean Journal of Pain, 30(1), 44-50.
Check out these techniques and more in the Lower Body Home-Study Course
On sale this week only!
Save 25% off the Upper Body Course!
NEW! Enhanced video USB format!!!
Learn unique approaches to work with the shoulder girdle, arms, neck, and torso, this course will prepare you to relieve painful myoskeletal issues in the upper body. Through video demos and animation, you’ll learn to identify several compensatory movement patterns and their associated reflexogenic pain. With this understanding of where the true source of problems arise, you’ll be able to develop highly effective treatment protocols and deliver lasting results. This course provides you with the skills you need to confidently relieve pain issues in the upper body. (20 CE)
Bonus: When you order the Home Study version, get the eLearning course and and an additional 2CE Ethics eCourse for free!
Save 25% off the Upper Body Course this week only. Offer expires Sunday, March 1st. Click the button below for more information and to purchase the course for CE hours and a certificate of completion to display in your office.








