Techniques as demonstrated in Technique Tour course.
The plantar fascia is far more than a tough sheet of connective tissue stretching from the heel bone to the toes. It’s part of an elegant spring-loaded system that makes human walking and running possible. When this system breaks down through injury, overuse, or too much “support”, painful conditions like plantar fasciosis can develop.
Anatomy of the Plantar Fascia
The plantar fascia (or plantar aponeurosis) originates at the medial calcaneal tubercle and fans forward to insert into the bases of the toes. It forms the deep structural floor of the arch, supporting and connecting the bones of the foot much like the cables of a suspension bridge.
Underneath lie the intrinsic muscles of the foot (including the flexor digitorum brevis, abductor hallucis, and quadratus plantae) which provide fine-tuned adjustments during stance and gait. Together, the fascia and these small muscles work as part of a tensegrity system that stores and releases elastic energy with each step.
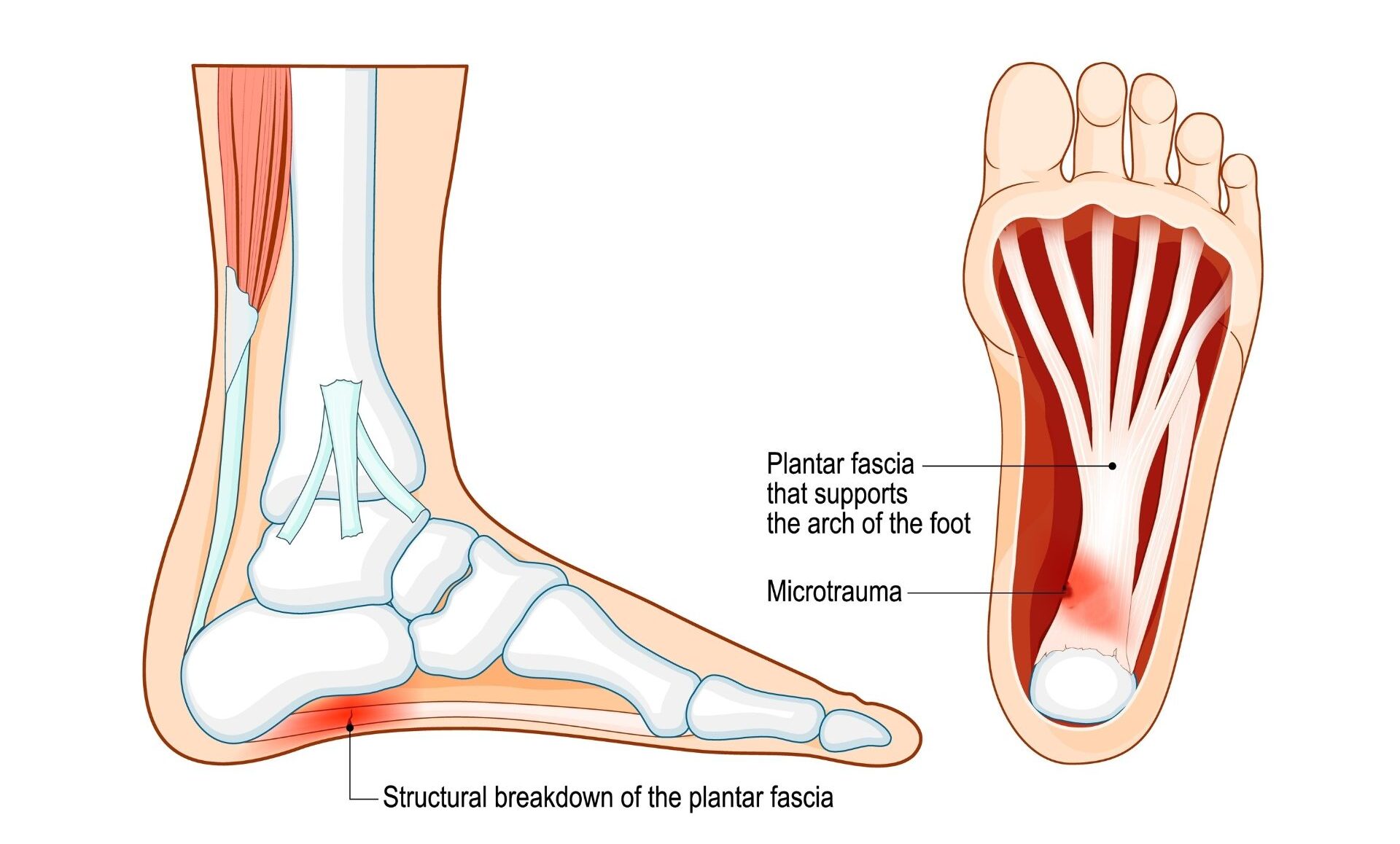
The plantar fascia and underlying muscles are part of an eloquent tensegrity spring system that uses a windlass mechanism to effectively absorb shock and spring us upward and onward.
Fasciitis or Fasciosis?
For years, people thought heel pain from this condition came mostly from inflammation. But research using imaging and tissue samples showed very little actual inflammation in most chronic cases. Instead, what’s really going on is microscopic tearing, poor healing, and degeneration of the fascia. The collagen fibers are fraying, not inflamed. So “fasciosis” is more accurate for long-term, chronic plantar pain. The “-itis” label fits better for an early, acute flare-up with short-term inflammation.
The Windlass Mechanism: Nature’s Shock Absorber
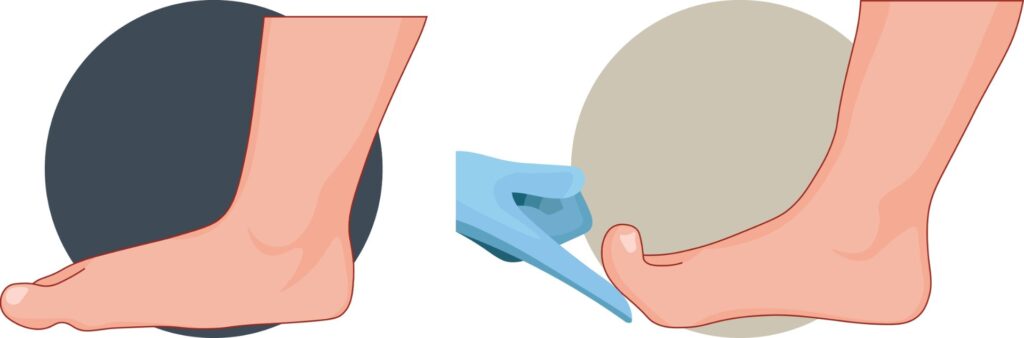
When we walk, the foot acts as both a mobile adapter and a rigid lever. During heel strike, the arch slightly collapses (pronation) to absorb impact. As we roll forward and the toes dorsiflex during push-off, the plantar fascia tightens—a process known as the windlass mechanism.
Imagine winding a winch: as the toes lift, the fascia wraps around the metatarsal heads, raising the arch and stabilizing the foot for propulsion. This transformation from flexible shock absorber to powerful springboard allows the lower body to recycle kinetic energy instead of losing it to the ground.
When the System Fails
Plantar fasciosis (formerly called plantar fasciitis) develops when this load-sharing mechanism breaks down. The tissue degenerates rather than inflames, often due to chronic overload and poor mechanics (Lemont et al., 2003).
In a healthy gait, the arch elevator muscles (tibialis anterior, peroneus longus, and tibialis posterior) coordinate with the plantar-flexors (gastrocnemius and soleus) to absorb and release energy smoothly. But when gait is altered through inactivity, rigid shoes, or excessive cushioning, the fascia and muscles lose their dynamic relationship.
Cushioned, arch-supporting footwear may seem protective, but it can reduce proprioceptive feedback and weaken intrinsic foot muscles over time. Studies show that children who grow up wearing structured shoes have a higher incidence of flat feet and plantar fasciosis later in life (Rao & Joseph, 1992). Our protective shoes, with all their arch support, may actually be the root cause for why a ballooning proportion of Americans suffer from flattened arches and plantar fasciosis. As the arches weaken, knees and hips begin to compensate, creating a cascade of joint strain up the kinetic chain.
The Barefoot Debate
Should we all toss our sneakers? Not so fast. Research on barefoot and minimalist running is still mixed. Forefoot striking can reduce impact on the knees and hips (Lieberman et al., 2010), but it may increase load on the Achilles tendon and plantar fascia, especially on hard urban surfaces.
While there’s no one-size-fits-all solution, there’s growing evidence that reconnecting with natural surfaces, like grass, sand, soil, can restore the body’s innate sense of balance and foot strength. You don’t need to run barefoot marathons to benefit. Simply walking, playing, or training without shoes for short periods allows the plantar fascia and intrinsic muscles to do the job nature intended.
Our feet evolved to move freely, to sense the ground, and to respond dynamically to changing terrain. By occasionally trading cushioned shoes for natural surfaces, we help preserve that uniquely human mode of transportation that’s been propelling us forward for millions of years.

Myoskeletal Perspective: Restoring Spring and Balance
In Myoskeletal Alignment Techniques (MAT), we view the foot as the foundation for the body’s kinetic chain. When the arch collapses or the plantar fascia loses elasticity, everything above—knees, hips, and even spinal alignment—must adapt.
Effective treatment goes beyond local soft-tissue work on the sole. It involves assessing five key dimensions of soft tissue function:
- Tissue texture: Detecting fibrosis, thickening, or nodular changes in the fascia.
- Tissue tension: Balancing the tonic and phasic muscle groups that influence arch height.
- Tissue movement: Restoring glide between fascial layers and joint play in the tarsal bones.
- Tissue function: Evaluating how the foot participates in gait and load transfer.
- Tissue neurology: Re-educating proprioceptive pathways so the brain re-learns efficient foot use.
Myoskeletal mobilization and proprioceptive retraining, combined with simple activities like mini-trampoline rebounding or barefoot walking on natural surfaces, help restore elasticity and coordination throughout the fascial web.

Why Therapists Should Care
Every step your client takes reflects the integrated behavior of bones, fascia, and brain. Weak or supported arches can silently shape posture, movement, and even chronic pain patterns far from the feet.
Understanding how the plantar fascia participates in whole-body tensegrity gives therapists a framework for assessing and treating pain from the ground up. Whether you’re working locally to decompress the fascia or globally to retrain postural balance, the goal is the same: restore the body’s ability to load, store, and release energy efficiently.
In Summary
Heeled and highly cushioned shoes may protect us from sharp objects, but they can rob the feet of strength, proprioception, and natural propulsion. Over time, the body recruits “anatomical reinforcements” (like the knees, hips, and spine) to make up for lost spring at the base. The result is fatigue, stiffness, and inefficient movement throughout the kinetic chain.
Treating plantar fasciosis isn’t just about easing heel pain, it’s about retraining the entire foot-to-brain conversation. A thorough history, careful palpation, and thoughtful movement retraining can restore this ancient, elegant system that’s been carrying us forward for millions of years.
Resources
To learn more about fascial tensegrity and gait mechanics, explore Erik Dalton’s Motion is Lotion course or the Dynamic Lower Body course.
Stecco, C., Corradin, M., Macchi, V., Morra, A., Porzionato, A., Biz, C., De Caro, R. (2013). Plantar fascia anatomy and its relationship with Achilles tendon and paratenon. Journal of Anatomy, 223(6), 665–676.
Hicks, J.H. “The Mechanics of the Foot: II. The Plantar Aponeurosis and the Arch.” Journal of Anatomy 88 (1954): 25–30.
Caravaggi, Paolo, et al. “A dynamic model of the windlass mechanism of the foot: evidence for early stance phase preloading of the plantar aponeurosis.” Journal of Experimental Biology 212.15 (2009): 2491-2499.
Lemont, H., et al. “Plantar Fasciitis: A Degenerative Process (Fasciosis) without Inflammation.” J Am Podiatr Med Assoc 93.3 (2003): 234–237.
Rao, U.B., & Joseph, B. “The Influence of Footwear on the Prevalence of Flat Foot.” J Bone Joint Surg Br 74.4 (1992): 525–527.
Kelly, L.A., et al. “Intrinsic Foot Muscles Have the Capacity to Control Deformation of the Longitudinal Arch.” J R Soc Interface 11.93 (2014): 20131188.
Lieberman, D.E., et al. “Foot Strike Patterns and Collision Forces in Habitually Barefoot versus Shod Runners.” Nature 463 (2010): 531–535.
Warne, J.P., & Gruber, A.H. “Transitioning to Minimal Footwear: A Systematic Review of Methods and Injury Risk.” Br J Sports Med 51.3 (2017): 160–167.
Dalton, E. (2015). Advanced Myoskeletal Alignment Techniques: Practitioner Training Manual. Oklahoma City, OK: Freedom from Pain Institute. (Course manual, internal publication.)
On sale this week only!
Save 25% off the Upper Body Course!
NEW! Enhanced video USB format!!!
Learn unique approaches to work with the shoulder girdle, arms, neck, and torso, this course will prepare you to relieve painful myoskeletal issues in the upper body. Through video demos and animation, you’ll learn to identify several compensatory movement patterns and their associated reflexogenic pain. With this understanding of where the true source of problems arise, you’ll be able to develop highly effective treatment protocols and deliver lasting results. This course provides you with the skills you need to confidently relieve pain issues in the upper body. (20 CE)
Bonus: When you order the Home Study version, get the eLearning course and and an additional 2CE Ethics eCourse for free!
Save 25% off the Upper Body Course this week only. Offer expires Sunday, March 1st. Click the button below for more information and to purchase the course for CE hours and a certificate of completion to display in your office.