Often, the patella is tilted and sits in the knee the way a beret rests on the side of one’s head, thus the term “squinting patella”. (Image 1.)
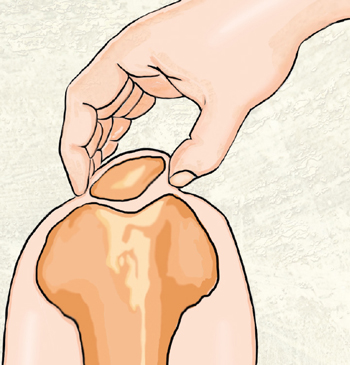
This abnormal positioning of the patella is a possible source of non-specific knee pain, and it can be caused by postural faults, including:
- knock-knees (genu valgum)
- bowed legs (genu varum)
- fallen arches (excessive pronation)
- high arches (excessive supination)
(Image 2.)
We’ve seen how pronated feet can wreak havoc on the knees as strong valgus shearing forces strain tendons, cartilage, and ligamentous tissues. Conversely, reduced shock absorption from high-arched feet can compensate up the kinetic chain causing a varus (bowlegged) shear force through the knees. In time, this abnormal ankle alignment disrupts the tibiofemoral joint’s antigravity function.
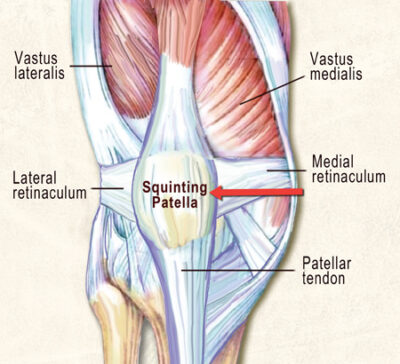
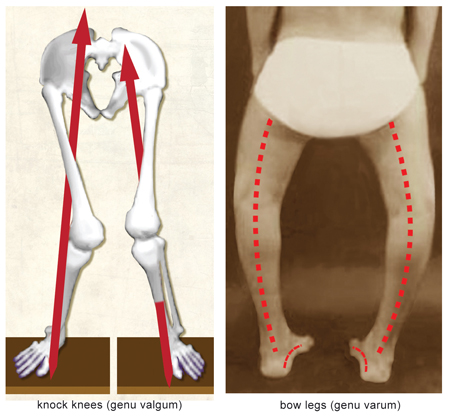
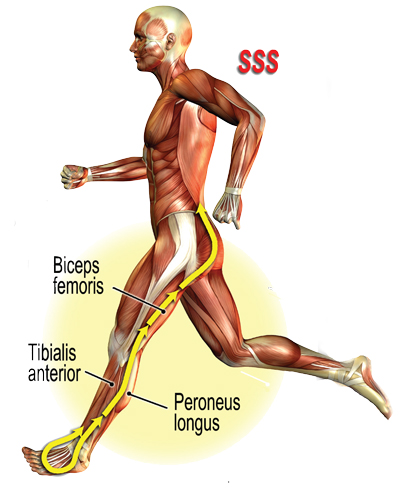
During clinical assessment we commonly see a squinting patella co-present with a chronically elongated medial and a tight lateral knee retinaculum. (Image 3. ) This sturdy retinacular band provides a perfect anchor for musculofascial attachments; therefore, it is most vulnerable to length-strength imbalances in and around the hip, leg, and foot. During gait, the slightest abnormality in the foot and ankle’s stirrup spring system (SSS) can alter antigravity function, resulting in knee and hip compensations. (Image 4.) In the presence of prolonged foot pronation, many global and core muscles forget how to “turn on” and “shut off” in proper sequence. Faulty peripheral input leads to faulty cortical processing and altered motor output. Meanwhile, the cerebellum valiantly attempts to correct the person’s coordination and balance problem by triggering spinal reflexes and accompanying reactive muscle guarding.
Guarding reflexes
Actual or perceived tissue injury due to overuse, underuse or plain old abuse can trigger spinal reflexes, resulting in:
- musculofascial splinting
- abnormal motor recruitment
- synergistic muscle dominance
- local or systemic inflammation
These effects can, in turn, trigger Movement Pattern Dysfunctions (MPDs).
Movement Pattern Dysfunctions
Simply stated, MPDs are imbalances in the movement of our bodies and present another complicating factor in knee pain assessment. MPDs can be large. They can be small. They can cause or be caused by knee pain. If someone limps, her brain is adapting MPDs to avoid further injury, while simultaneously allowing the body to carry on with daily living.
MPDs are complex, motor-learned programs ultimately governed by the brain. These ingrained faulty movement patterns develop from muscle imbalances, joint restrictions, poor stability, or previous injury. In those clients presenting with runner’s knee, there may be multiple biomechanical imbalances at play. The most common involve the hip and ankle joints. So, instead of directing treatment to the knee itself, I first assess and treat MPDs originating at the client’s hips, ankles or feet and then address knee alignment and mobility issues as shown in the Log Roll technique demonstrated in the video and described below.
MAT therapy, along with a well-designed and executed corrective exercise program, helps restore and maintain the movement quality of joints. Ultimately, this treatment will reduce MPDs, and permit the body’s natural healing processes to restore function in those clients with runner’s knee pain.
Ida Rolf Log Roll
GOAL: Internally rotate client’s externally rotated femur
LANDMARK: Musculofascia of client’s extremely rotated femur
ACTION:
- Standing on client’s right side, therapist’s right hand comes under client’s femur and internally rotates client’s entire leg
- Therapist places his left hand on top of client’s thigh to provide leverage to further internally rotate her leg
- Therapist asks client to gently externally rotate her thigh against his resistance to a count of five and relax
- Therapist’s hands bring client’s femur and hip into greater internal rotation
- Repeat 3 to 5 times for improved alignment and function
On sale this week only!
Save 25% off the Upper Body Course!
NEW! Enhanced video USB format!!!
Learn unique approaches to work with the shoulder girdle, arms, neck, and torso, this course will prepare you to relieve painful myoskeletal issues in the upper body. Through video demos and animation, you’ll learn to identify several compensatory movement patterns and their associated reflexogenic pain. With this understanding of where the true source of problems arise, you’ll be able to develop highly effective treatment protocols and deliver lasting results. This course provides you with the skills you need to confidently relieve pain issues in the upper body. (20 CE)
Bonus: When you order the Home Study version, get the eLearning course and and an additional 2CE Ethics eCourse for free!
Save 25% off the Upper Body Course this week only. Offer expires Sunday, March 1st. Click the button below for more information and to purchase the course for CE hours and a certificate of completion to display in your office.