From Dynamic Lower Body course
Myoskeletal technique for hip and back pain
In the early 20th century, sacroiliac joint syndrome (SIJ) was the most common medical diagnosis for low back pain, which resulted in that period being labeled the “Era of the SI Joint.” Any pain emanating from the low back, buttock or adjacent leg usually was branded and treated as SIJ. However, this medical mindset came to a screeching halt in 1934, when Jason Mixter, MD, published an article on the intervertebral disc in The New England Journal of Medicine.1His landmark report challenged the popular understanding of sciatica and helped establish surgery’s prominent role in the management of sciatica at the time. Throughout the years, discectomy surgery has increased in popularity, causing many to define this period as “Dynasty of the Disc.”


Femoroacetabular, SI and Lumbar Spinal Joints
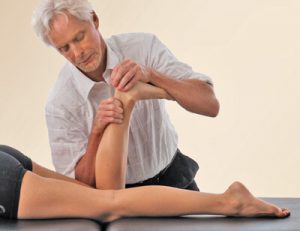
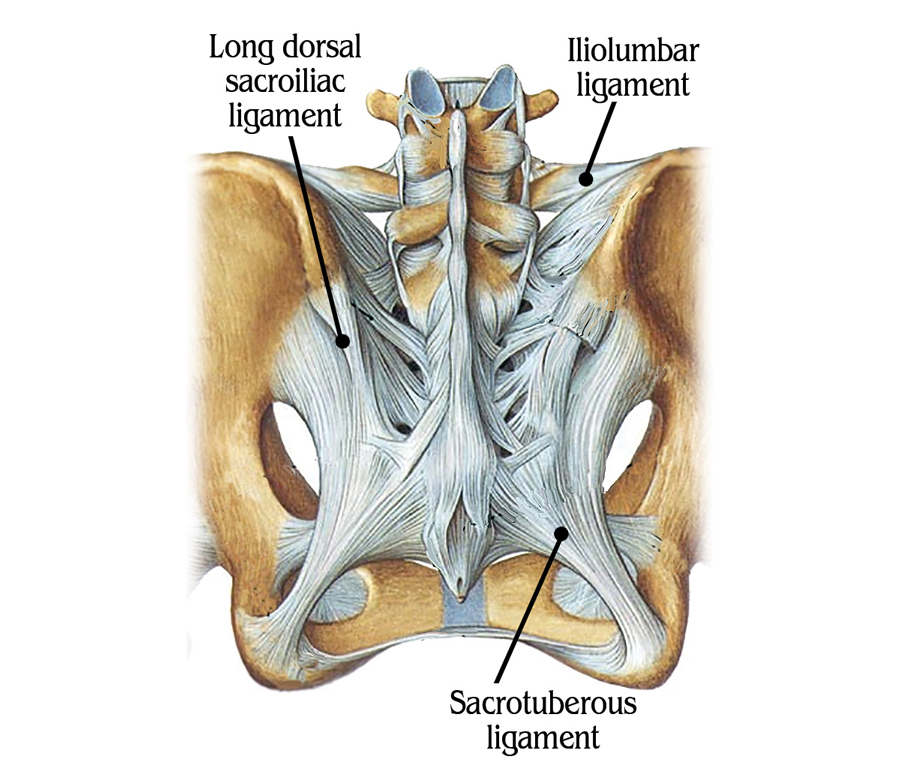
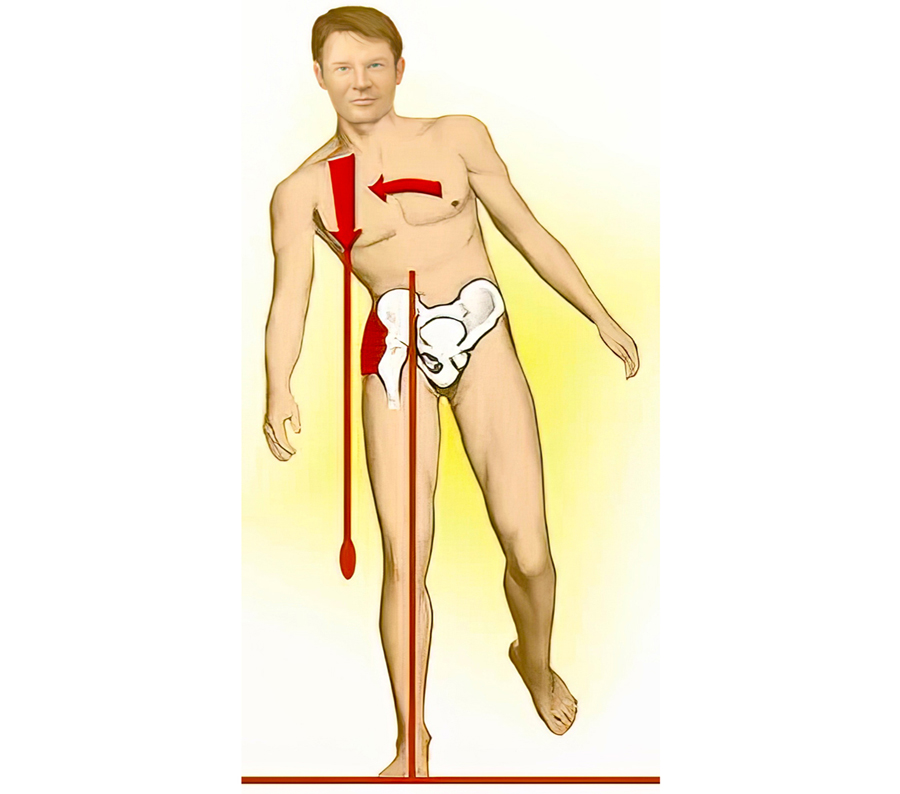
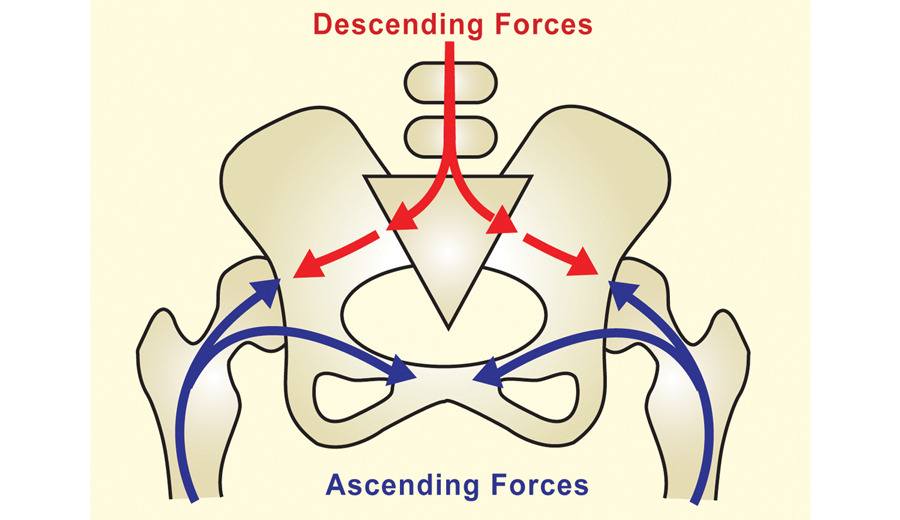
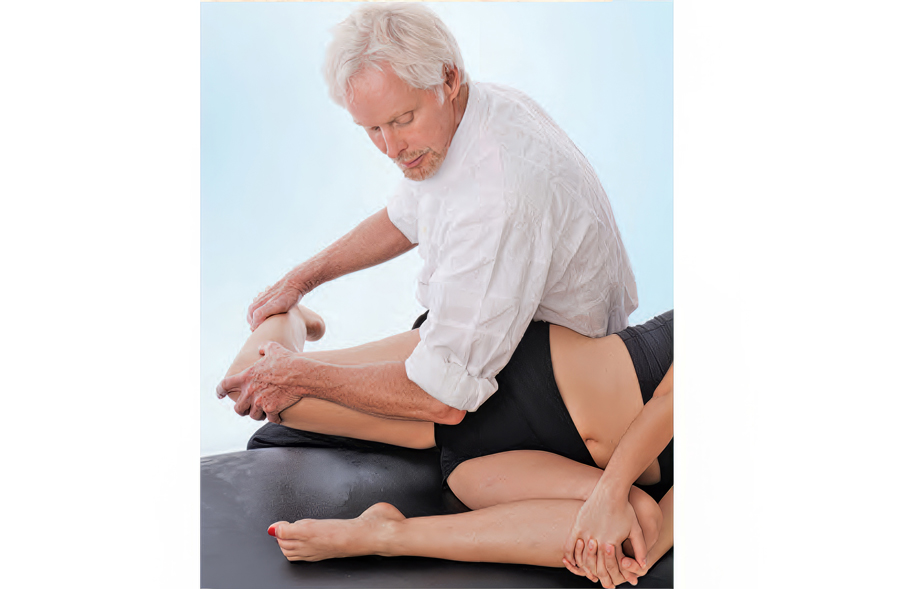
Although the three bones of the pelvis frequently are at the seat of a “primary” lesion, I’ve found that a missing key in successful correction of SI pain is mobilizing motion-restricted femoroacetabular (hip) joints. For the pelvis to effectively absorb the forces imposed upon it, the hips must be aligned and functioning properly. Normally, it’s not the gross motions creating dysfunction within the hip’s truncated joint capsule, but restrictions of minor movements caused by such things as iliofemoral ligament adhesions (Image 6.). Therefore, a rational treatment approach would begin with mobilization of the adhesive anterior hip capsule as shown in Image 7., followed by the iliosacral and sacroiliac alignment techniques presented above.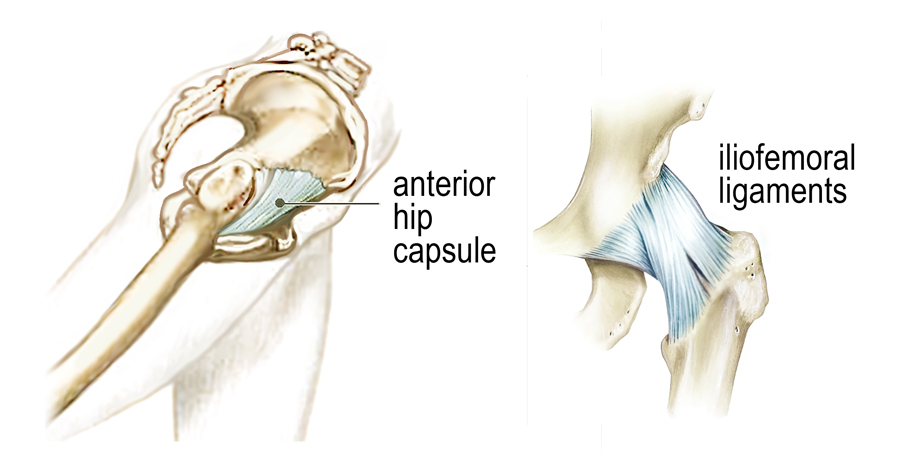
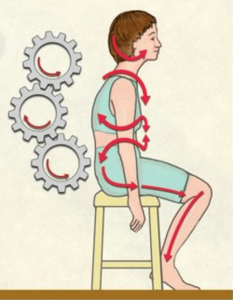
Legendary neurologist and physiotherapist Vladimir Janda, MD, reminds us that: “Any alteration in joint function caused by capsular restriction or loss of joint play affect muscles that cross the dysfunctional joint either through inhibition (weakening) or facilitation (tightening).” Many in today’s flexion-addicted society suffer from anterior hip capsule adhesions and tight iliopsoas muscles that bind the right femur into a flexed position, preventing adequate hip extension during gait. Yet we have to walk … so what happens biomechanically? As the right leg swings back into extension, the neurologically shortened iliopsoas and fibrosed right hip capsule prevent full hip extension causing the pelvic bowl to anteriorly rotate. This results in facet joint and disc compression, overstretching of pelvic ligaments, and compensatory lumbar scoliosis.
Summary
A stable pelvis is achieved through proper upper and lower quadrant balance and is essential for long-term low back and SI joint health. In the presence of pelvic instability, the brain will attempt to stabilize the lumbosacral joint by layering the area with protective spasm, but it does little good for therapists to try and release the muscle hypertonicity until the hip and pelvic alignment problems are corrected. Myoskeletal techniques that include low-force mobilization and graded-exposure stretching help the brain recognize and reorganize neural input resulting in less reactive muscle spasm, less pain and happier clients.
References
- Parisien RC, Ball PA. William Jason Mixter (1880-1958). Ushering in the “dynasty of the disc.” Spine 1998;23(21):2363-6.
- Janda V. Treatment of chronic back pain. Journal of Manual Medicine1992;6:166-8.
On sale this week only!
Save 25% off the "Dalton Technique Treasures" eCourse
The “Dalton Technique Treasures” eLearning course is a compilation of some of Erik’s favorite Myoskeletal Alignment Techniques (MAT). Learn MAT techniques to assess and address specific sports injuries, structural misalignment, nervous system overload, and overuse conditions. ON SALE UNTIL July 29th! Get Lifetime Access: As in all our eLearning courses, you get easy access to the course online and there is no expiry date.